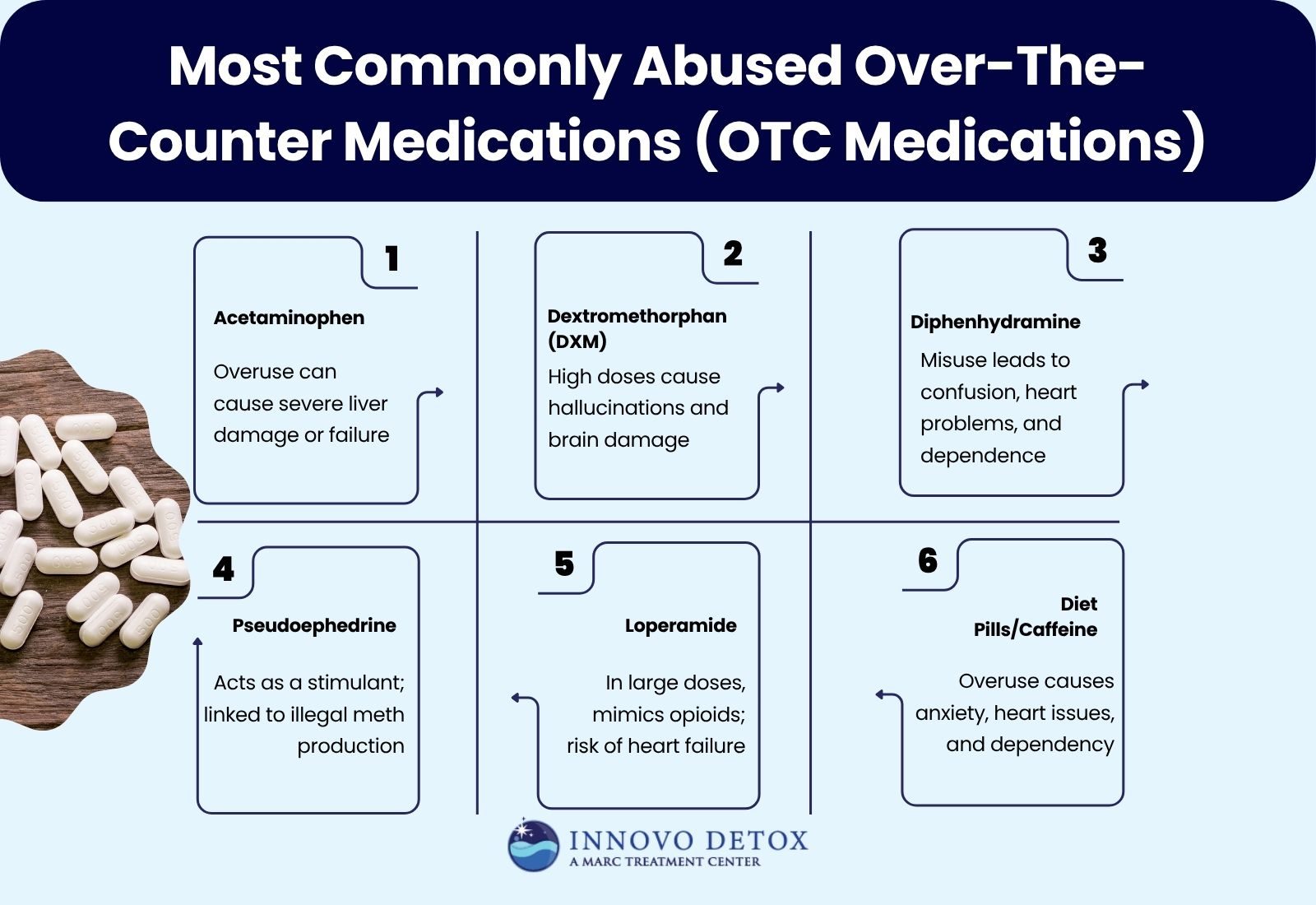
The most commonly abused over-the-counter (OTC) medications are those that people misuse for pain relief, sleep aid, or stimulant effects without realizing their potential for addiction or serious health risks. These include everyday drugs like acetaminophen, dextromethorphan (DXM), diphenhydramine, pseudoephedrine, loperamide, and diet or caffeine-based supplements.
In Pennsylvania, nearly 7% of substance misuse cases involve OTC medications, reflecting a concerning trend of dependency on readily available drugs. While these products are safe when used as directed, excessive or nonmedical use leads to liver damage, cardiac arrest, and severe withdrawal symptoms.
Recognizing the dangers of OTC misuse is vital to preventing long-term harm. Professional detox and treatment programs in Pennsylvania help individuals recover safely, while family involvement strengthens emotional support.
Below are the most frequently misused over-the-counter medications:
1. Acetaminophen (Tylenol)
Acetaminophen is one of the most used OTC drugs in America, primarily for pain relief and fever reduction. However, when taken in excessive doses, it causes severe liver damage or liver failure.
Every year, approximately 60,000 Americans are hospitalized due to an acetaminophen overdose, from accidental misuse or during a mental health crisis. Chronic overuse elevates liver enzyme levels, reduces the liver’s ability to filter toxins, and, in extreme cases, results in fatal outcomes.
2. Dextromethorphan (DXM) – Found in Cough Syrups Like Nyquil or Robitussin
Dextromethorphan, or DXM, is a cough suppressant found in many cold and flu medications. In low doses, it safely relieves coughs. In high doses, it acts as a dissociative hallucinogen, producing euphoric or mind-altering effects similar to ketamine or PCP.
Misuse of DXM, referred to as robotripping, causes hallucinations, rapid heartbeat, paranoia, and brain damage. Due to increasing misuse, over 20 U.S. states have enacted restrictions on the sale of DXM-containing cough syrups to minors.
3. Diphenhydramine (Benadryl)
Diphenhydramine, an antihistamine used to treat allergies and insomnia, causes sedation and mild euphoria when taken in higher-than-recommended doses. Abuse of Benadryl leads to confusion, rapid heart rate, hallucinations, and memory impairment.
Chronic misuse of Benadryl also causes dependency and severe withdrawal symptoms upon discontinuation. In some cases, diphenhydramine abuse has been linked to cardiac arrhythmia and seizures.
4. Pseudoephedrine and Phenylephrine (Sudafed)
Pseudoephedrine, commonly found in decongestants like Sudafed, relieves nasal congestion by narrowing blood vessels in the nasal passages. However, it also acts as a stimulant, producing increased alertness and euphoria when abused.
Historically, pseudoephedrine was used in the illegal manufacturing of methamphetamine, leading to strict purchasing regulations. Today, federal law limits how much pseudoephedrine is purchased in a single transaction, and pharmacies must record buyer information to prevent misuse.
5. Loperamide (Imodium A-D)
Loperamide is used to control diarrhoea by slowing intestinal movement. However, in very high doses, it produces opioid-like effects, including sedation and pain relief. Because it acts on the same brain receptors as opioids, individuals struggling with opioid withdrawal sometimes misuse it to ease symptoms.
Large doses of loperamide lead to cardiac arrest, intestinal blockages, and death. The FDA has issued warnings about the dangers of high-dose loperamide use, urging consumers to follow label directions strictly.
6. Diet Pills and Caffeine Supplements
Diet pills and caffeine-based OTC products are misused for weight loss or energy boosts. Both overstimulate the central nervous system, causing increased heart rate, insomnia, anxiety, and dependency.
In extreme cases, diet pills and caffeine-based OTC products trigger cardiac arrhythmias or high blood pressure. Many diet pills previously contained ephedrine, a stimulant banned by the FDA due to severe cardiovascular risks.
Nevertheless, unregulated supplements containing ephedra derivatives are still available online. Individuals with eating disorders or substance use disorders are particularly vulnerable to these forms of OTC abuse.
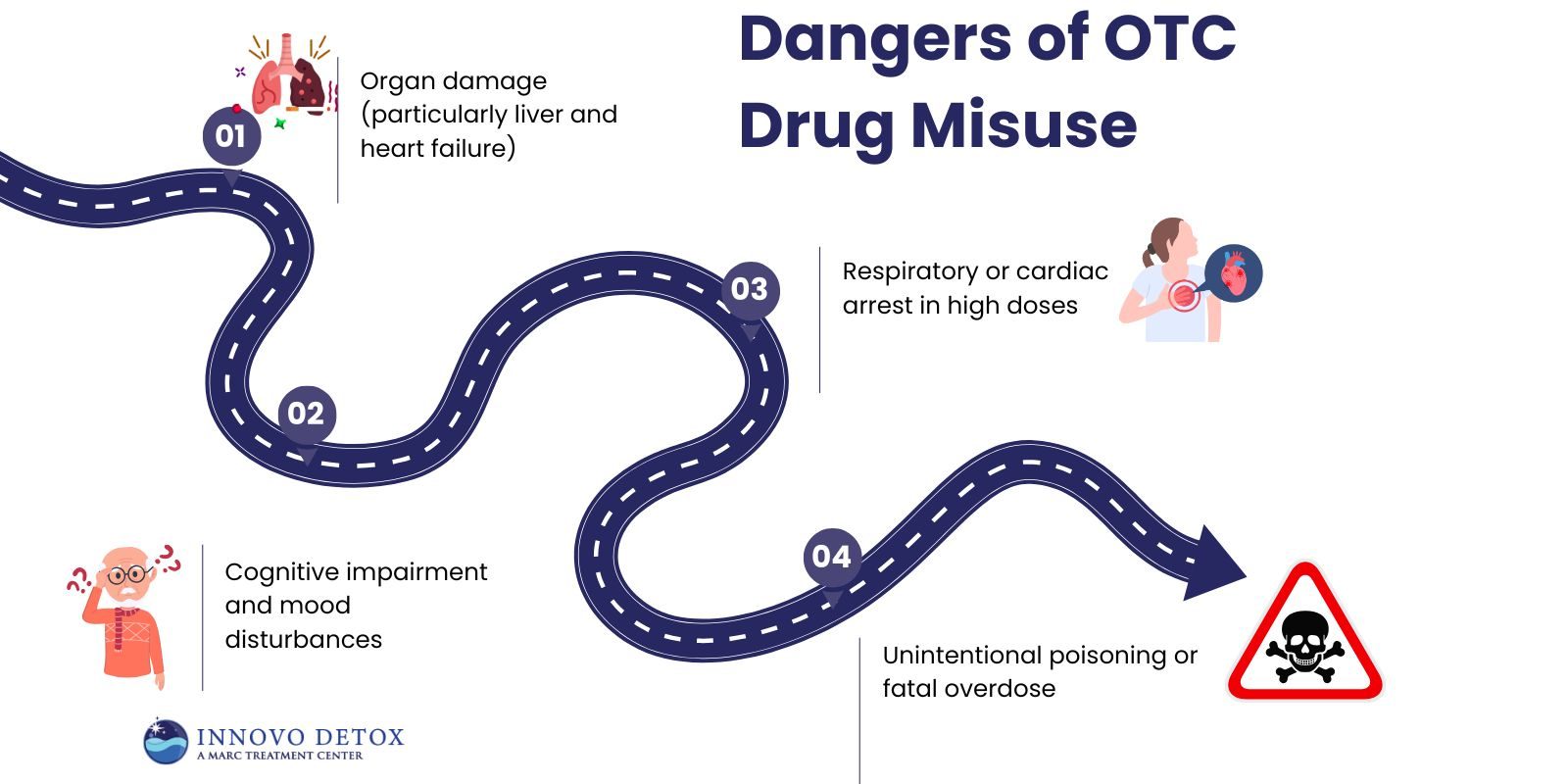
What Are the Dangers of OTC Drug Misuse?
The dangers of OTC drug misuse include increasing the risk of addiction, overdose, and long-term health complications. Unlike prescription drugs, OTC products are viewed as harmless, leading people to underestimate their risks.
The dangers of OTC drug misuse include:
- Organ damage (particularly liver and heart failure)
- Cognitive impairment and mood disturbances
- Respiratory or cardiac arrest in high doses
- Unintentional poisoning or fatal overdose
The FDA emphasizes that consumers must always read dosage instructions carefully, avoid mixing OTC drugs with alcohol or other medications, and consult healthcare professionals if symptoms persist beyond the expected duration.
What Should You Do If You Suspect OTC Medication Abuse in Pennsylvania?
If you or someone you know is showing signs of OTC medication abuse, such as needing higher doses to feel relief, taking OTC drugs for non-medical effects, or hiding use, it’s important to seek professional help in Pennsylvania.
Detoxification and clinical stabilization programs manage withdrawal safely and prepare individuals for further treatment. Facilities in Pennsylvania provide medically supervised detox programs that address both physical withdrawal and the underlying psychological aspects of substance misuse. Their approach ensures that individuals safely transition from detox into long-term recovery support.
How Do Family Dynamics and Detox Influence the Recovery Process?
Family dynamics and detox influence the recovery process by shaping the emotional and psychological environment that supports or hinders healing. A stable, understanding family can reduce stress, encourage adherence to treatment, and provide accountability during withdrawal and early recovery.
Unresolved conflicts or codependent relationships can trigger relapse and emotional instability. Open communication, therapy involvement, and education for family members improve overall outcomes. When families actively participate in treatment, both the individual and their loved ones begin healing together, highlighting how Family Dynamics and Detox are deeply interconnected in achieving sustainable recovery.