Outpatient alcohol rehab provides structured treatment for alcohol use disorder (AUD) without requiring patients to stay at a residential facility. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), outpatient rehab allows individuals to receive therapy sessions, develop coping strategies, and maintain their daily responsibilities, which are crucial for long-term recovery.
The process of outpatient alcohol rehab starts with a comprehensive assessment of alcohol use, followed by the development of a personalized recovery plan. Patients then attend therapy sessions, typically 1–5 times a week, which include individual therapy, group counseling, and family support, while also participating in aftercare programs.
Types of Outpatient alcohol rehab include Standard Outpatient Programs (OP), Intensive Outpatient Programs (IOP), and Partial Hospitalization Programs (PHP).
The key benefits of outpatient alcohol rehab are its flexibility, affordability, and the ability to integrate recovery into daily life. A study by the National Institute on Drug Abuse (NIDA) shows that outpatient rehab helps individuals maintain work, school, and family obligations while providing structured therapy to prevent relapse.
Major treatment approaches in outpatient rehab include Cognitive-Behavioral Therapy (CBT), Motivational Interviewing (MI), and Medication-Assisted Treatment (MAT). These approaches target thought patterns, enhance motivation, and provide pharmacological support.
The average cost of outpatient alcohol rehab in the U.S. ranges from $1,000 to $10,000 for a 30-day program, depending on the type of program and level of care required. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), outpatient programs are more affordable compared to inpatient rehab, which costs between $6,000 and $20,000 for a 30-day stay.
What is Outpatient Alcohol Rehab?
Outpatient alcohol rehab is a structured, part-time treatment program designed to support individuals in alcohol recovery without requiring overnight stays in a facility. Unlike inpatient rehab, where patients live on-site and follow intensive daily routines, outpatient programs allow participants to live at home and maintain their daily responsibilities while receiving treatment.
According to the National Institute on Drug Abuse (NIDA), approximately 40% of individuals seeking treatment for alcohol use disorder in the U.S. opt for outpatient rehab programs due to their flexible scheduling and accessibility. These programs are recommended for individuals with mild to moderate alcohol dependency or those transitioning from inpatient care.
The core purpose of outpatient rehab is to provide consistent therapy, monitoring, and support while allowing patients to integrate their recovery process into real-world environments. This model promotes long-term behavior change and relapse prevention while reducing disruption to work, school, or family life.
What Does an Outpatient Alcohol Rehab Program Consist of?
An outpatient alcohol rehab consists of therapy sessions, medical care, and support services delivered on a scheduled basis. These programs include individual counseling, group therapy, educational workshops, and access to relapse prevention tools—all within a flexible, part-time treatment structure.
The outpatient alcohol rehab program is explained below:
- Individual therapy sessions: One-on-one counseling helps clients uncover the root causes of alcohol use and build self-awareness. A structured recovery plan is developed collaboratively with a licensed therapist. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), individualized behavioral therapy improves alcohol abstinence outcomes by 27% in outpatient settings.
- Group counseling: Peer-led or professionally guided group discussions foster connection, reduce isolation, and allow the sharing of real-life challenges. Participants practice communication, accountability, and mutual support.
- Medical monitoring: Ongoing evaluations by healthcare professionals track withdrawal symptoms, medication use, and physical health. This ensures safety and early detection of relapse risks. According to a 2020 report by the Substance Abuse and Mental Health Services Administration (SAMHSA), outpatient programs with integrated medical oversight reduced hospital readmission by 18%.
- Lifestyle and coping strategies education: Clients receive training in stress management, emotional regulation, and relapse prevention. Skills are taught through workshops and assignments tied to real-life scenarios.
How Does Outpatient Alcohol Rehab Work?
Outpatient alcohol rehab works by following a structured process that includes therapy sessions, medical supervision, and regular progress assessments tailored to each individual’s recovery plan. Patients attend scheduled appointments multiple times a week while applying new coping strategies in their daily environment, reinforcing behavior change in real time.
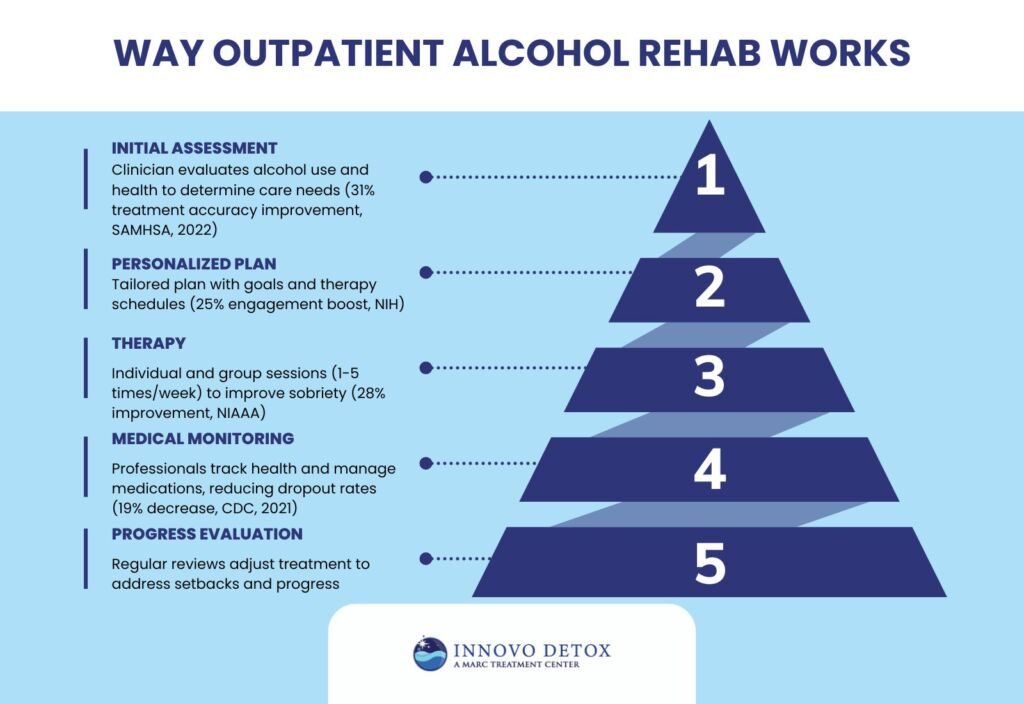
The way outpatient alcohol rehab works is explained below:
- Initial assessment and diagnosis: A licensed clinician conducts a comprehensive evaluation of alcohol use patterns, mental health status, and medical history. This step determines the appropriate level of care and identifies co-occurring disorders. According to SAMHSA (2022), proper assessment improves treatment accuracy by 31%.
- Creation of a personalized recovery plan: Based on assessment results, a tailored recovery plan is developed with input from the patient. It outlines therapy goals, session schedules, and support services. Research from the National Institutes of Health (NIH) shows that individualized planning improves engagement by 25%.
- Enrollment in therapy sessions: Patients attend individual and group therapy sessions to build awareness, manage triggers, and strengthen emotional regulation. Frequency ranges from 1 to 5 times per week, depending on program intensity. The NIAAA reports that consistent outpatient therapy contributes to a 28% improvement in sustained sobriety.
- Medical care and monitoring: Healthcare professionals oversee medication management (if used), track withdrawal symptoms, and monitor physical health. Regular check-ins ensure safety and prevent relapse. According to a 2021 CDC review, outpatient medical monitoring reduced treatment dropout rates by 19%.
- Ongoing progress evaluation: Therapists and case managers review patient progress biweekly or monthly to adjust treatment as needed. This ensures that setbacks are addressed early and successes are reinforced.
What Level of Commitment Is Required for Outpatient Alcohol Rehab to Be Effective?
The level of commitment required for outpatient alcohol rehab to be effective includes consistent attendance, personal dedication, and willingness to make lifestyle changes. Most programs require attending therapy sessions 3 to 5 times per week, with each session lasting 1 to 3 hours.
Patients must also actively engage in their recovery plan by completing assignments, attending support groups, and applying learned coping strategies in daily life. Success in outpatient rehab depends heavily on internal motivation, honesty during counseling, and establishing a stable environment that supports sobriety—especially since patients remain exposed to triggers and social pressures outside of treatment hours.
How Long Does an Outpatient Rehab Program Typically Last?
An outpatient alcohol rehab program lasts between 30 to 90 days, though some extend up to 6 months based on individual needs. Duration varies depending on the severity of alcohol use, progress during treatment, and the type of program—standard, intensive, or partial hospitalization.
Many facilities offer flexible schedules and customizable recovery plans to accommodate work, school, or family commitments, with regular evaluations guiding any extensions or adjustments.
What Aftercare Services Are Available After Completing Outpatient Alcohol Rehab?
The aftercare services available after completing outpatient alcohol rehab are ongoing therapy, relapse prevention planning, and support groups. These services help individuals maintain long-term sobriety by reinforcing coping strategies, monitoring progress, and providing consistent emotional and social support.
The aftercare services available after completing outpatient alcohol rehab are explained below:
- Relapse prevention programs: These structured services help individuals identify personal triggers and develop long-term coping strategies to avoid relapse. Programs include follow-up therapy, regular progress check-ins, and behavioral planning. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), structured relapse prevention reduces the risk of recurrence by 36% in outpatient graduates.
- Sober living homes: Transitional housing offers a substance-free environment with peer accountability and house rules that reinforce sober routines. Residents follow curfews, attend meetings, and undergo random alcohol testing.
- Continued counseling: One-on-one or group therapy continues post-treatment to strengthen emotional regulation, reinforce motivation, and address any setbacks. Many outpatient centers offer monthly or biweekly counseling options as part of their aftercare plans. The Substance Abuse and Mental Health Services Administration (SAMHSA) notes that ongoing counseling improves long-term recovery outcomes by 28%.
- Support groups: Peer-led groups such as Alcoholics Anonymous (AA) or SMART Recovery provide regular meetings, mentorship, and a shared sense of accountability. These groups help individuals stay grounded and connected to a sober community. A study by Stanford University’s School of Medicine (2020) showed that AA participation increased long-term sobriety rates by 20% to 40%, depending on meeting frequency.
What Types of Outpatient Alcohol Rehab Programs Are Available?
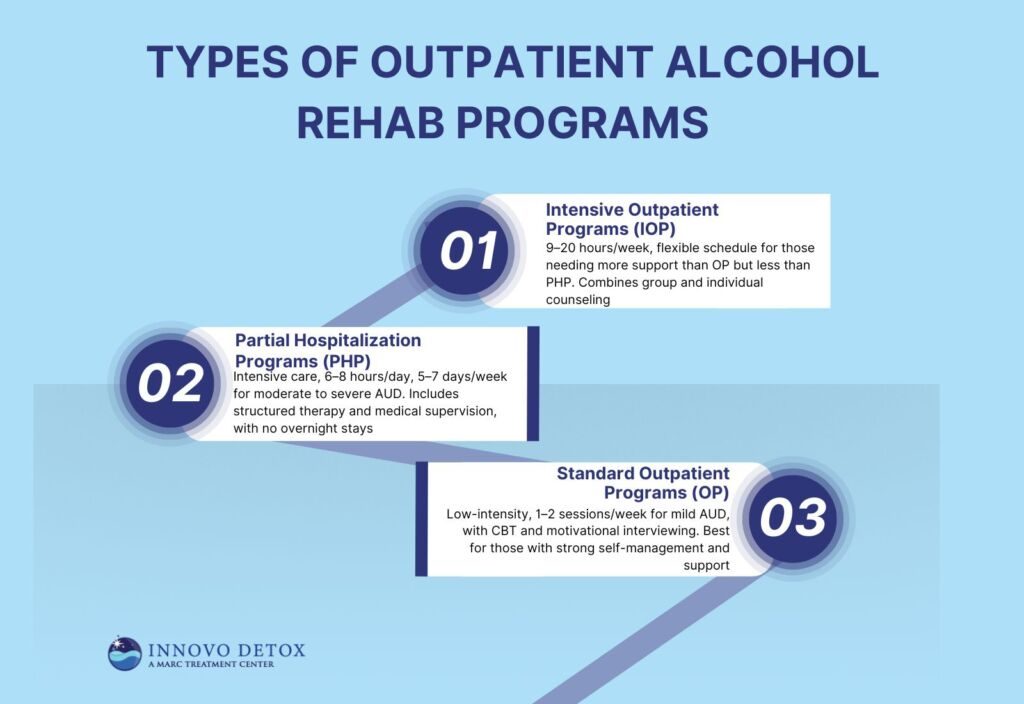
The types of outpatient alcohol rehab programs available include Standard Outpatient Programs (OP), Intensive Outpatient Programs (IOP), and Partial Hospitalization Programs (PHP). Each program varies in intensity, frequency of therapy sessions, and medical involvement, allowing individuals to choose based on the severity of their alcohol use and daily responsibilities.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2019, 43% of individuals seeking substance use treatment enrolled in standard outpatient programs, 13% participated in intensive outpatient programs, and 14% engaged in partial hospitalization programs.
The types of outpatient alcohol rehab programs available are explained below:
1. Standard Outpatient Programs
Standard Outpatient Programs (OP) are low-intensity alcohol rehab options designed for individuals with mild alcohol use disorder (AUD) who do not require constant supervision. These programs allow clients to continue daily activities while participating in scheduled therapy sessions, making them ideal for those with strong self-management skills and a stable home environment.
Key features of standard outpatient programs include:
- Session frequency: 1–2 sessions per week, each lasting 60–90 minutes.
- Therapy types: Includes cognitive-behavioral therapy (CBT), motivational interviewing, and occasional group therapy.
- Support needs: Patients benefit most when they have a reliable support system at home and access to community resources or peer groups.
2. Partial Hospitalization Programs (PHP)
Partial Hospitalization Programs (PHP) are day treatment options that offer intensive care for individuals with moderate to severe alcohol use disorder who require more support than traditional outpatient care but do not need 24-hour supervision.
PHPs deliver full-day structured therapy and medical supervision, lasting 6 to 8 hours per day, 5 to 7 days a week, while patients return home each evening. This model blends clinical oversight with flexibility, making it an effective step-down from inpatient care.
Key characteristics of PHPs include:
- Structured therapy: Daily sessions combining individual therapy, group counseling, and evidence-based treatment modules.
- Medical supervision: On-site professionals monitor withdrawal symptoms, medication adherence, and physical health.
- Behavioral counseling: Emphasis on identifying triggers, building coping strategies, and maintaining long-term recovery goals.
- No overnight stays: Unlike inpatient programs, PHPs allow patients to live at home, promoting real-world accountability.
3. Intensive Outpatient Programs (IOP)
Intensive Outpatient Programs (IOP) provide structured treatment for individuals who need more support than a Standard Outpatient Program (OP) but do not require the full-day intensity of a Partial Hospitalization Program (PHP). IOPs involve 9 to 20 hours of therapy per week, combining group therapy, one-on-one counseling, and workshops focused on relapse prevention and emotional regulation.
These programs offer a flexible schedule— during evenings or weekends—making them ideal for individuals balancing recovery with work or family responsibilities. IOPs are especially beneficial for those who need structured care without stepping into inpatient or full-day day treatment environments.
Is Online or Telehealth Outpatient Rehab for Alcohol Available?
Yes, online or telehealth outpatient rehab for alcohol is available. Virtual programs offer remote access to individual counseling, group therapy, relapse prevention planning, and progress monitoring through secure video platforms.
These services are designed for people who need flexibility due to distance, work schedules, or mobility issues while still participating in structured recovery plans. According to a study by Karen E. Johnson titled “Effectiveness of Telehealth Services in Substance Use Treatment,” published in Psychiatric Services (2021), virtual addiction care produced comparable outcomes to in-person treatment, with no significant difference in relapse rates or therapy adherence.
What Are the Benefits of Outpatient Alcohol Rehab?
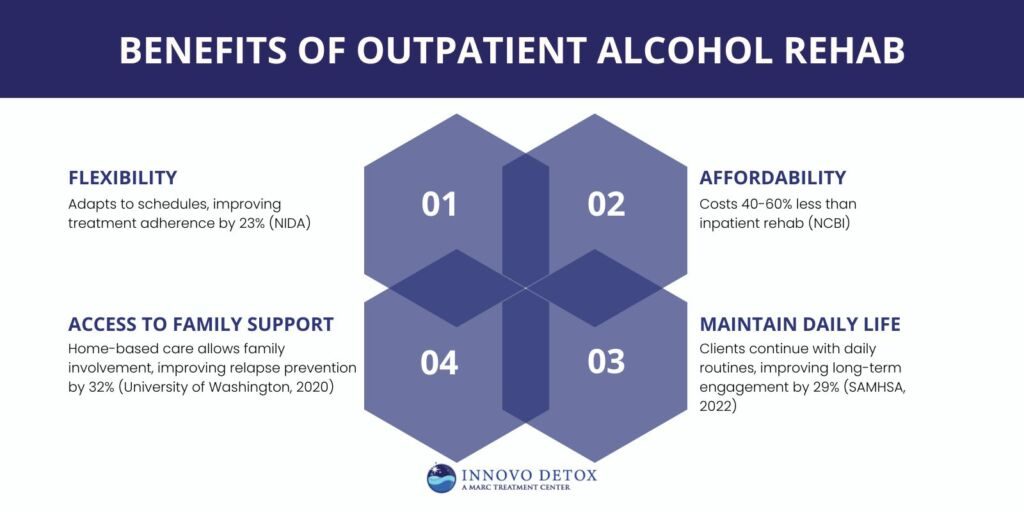
The benefits of outpatient alcohol rehab are flexibility, affordability, and real-world recovery integration. Patients maintain work, family, and school responsibilities while receiving structured therapy at a lower cost than inpatient care, and practice their coping strategies in real-time environments.
The benefits of outpatient alcohol rehab are explained below:
- Flexibility: Outpatient rehab offers adaptable scheduling, allowing individuals to attend therapy sessions during evenings or weekends. This structure is ideal for those managing work, school, or caregiving responsibilities. According to the National Institute on Drug Abuse (NIDA), flexible scheduling in outpatient care improves treatment adherence by 23%.
- Affordability: These programs typically cost significantly less than inpatient rehab as they don’t require housing, meals, or 24-hour care. Sliding scale fees and insurance coverage also make outpatient care more accessible. A report by the National Center for Biotechnology Information (NCBI) found that outpatient rehab reduces treatment costs by 40% to 60% compared to residential programs.
- Ability to maintain daily life: Clients can continue living at home and meeting personal obligations while undergoing structured therapy. This helps reduce stigma and promotes the immediate application of recovery skills. According to SAMHSA (2022), maintaining life routines during treatment improves long-term engagement by 29%.
- Access to family support: Being home-based allows individuals to receive emotional and logistical support from loved ones. Many programs also involve family in counseling and education sessions. A study by the University of Washington Department of Psychology (2020) reported that family involvement in outpatient rehab improves relapse prevention outcomes by 32%.
What Treatment Approaches are Used in Outpatient Rehab for Alcohol?
The treatment approaches used in outpatient rehab for alcohol are cognitive-behavioral therapy (CBT), motivational interviewing (MI), and medication-assisted treatment (MAT). These methods target thought patterns, enhance motivation for change, and manage cravings—offering a well-rounded approach to long-term alcohol recovery.
The treatment approaches used in outpatient rehab for alcohol are explained below:
- Individual Therapy: Individual therapy involves private sessions with a licensed therapist to address personal triggers, co-occurring mental health issues, and emotional challenges tied to alcohol use. This method forms the foundation of a tailored recovery plan and allows for in-depth progress tracking. It supports self-awareness, behavioral change, and long-term goal setting. According to a study by Linda M. Sobell titled “Individualized Treatment for Alcohol Use Disorders,” published in the Journal of Substance Abuse Treatment (2020), individual therapy increased treatment retention by 30%.
- Group Counseling: Group counseling promotes peer support, shared accountability, and connection through therapist-led discussions. It reduces isolation and helps patients develop social coping strategies. Group settings also give participants exposure to different perspectives and recovery techniques. According to a study by James R. McKay titled “Group Therapy Outcomes in Outpatient Settings,” published in the American Journal of Drug and Alcohol Abuse (2019), participants in group counseling reported a 40% improvement in relapse prevention outcomes.
- Family Therapy: Family therapy integrates loved ones into the recovery process to rebuild trust, improve communication, and address enabling behaviors. Sessions educate families about addiction and teach support methods for sustaining sobriety. This approach is especially valuable when the home environment directly impacts relapse risk. According to a study by William Fals-Stewart titled “Behavioral Family Counseling for Alcohol Abuse,” published in NIAAA Clinical & Research Studies (2017), family therapy increased successful recovery outcomes by 26%.
- Cognitive-Behavioral Therapy (CBT): CBT helps patients recognize distorted thinking patterns and replace them with healthier beliefs and behaviors. In outpatient settings, it focuses on stress regulation, relapse prevention, and problem-solving skills. CBT is one of the most evidence-supported approaches in alcohol treatment. According to a study by Kathleen M. Carroll titled “Cognitive-Behavioral Therapy for Substance Use Disorders,” published in Psychiatry Research (2018), CBT reduced relapse rates by 35%.
- Motivational Interviewing (MI): MI is a collaborative counseling style that strengthens a person’s motivation and commitment to change. It helps patients resolve ambivalence and actively engage in the recovery process. This method is especially effective in early-stage treatment. According to a study by William R. Miller titled “Motivational Interviewing in Treating Substance Abuse,” published in the Journal of Clinical Psychology (2017), MI improved patient motivation and engagement by 48%.
- Medication-Assisted Treatment (MAT): MAT combines FDA-approved medications with behavioral therapy to manage cravings, reduce withdrawal, and prevent relapse. Common medications include naltrexone, acamprosate, and disulfiram. MAT is integrated into outpatient care to stabilize physical symptoms while counseling addresses emotional triggers. According to a study by Nora D. Volkow titled “Effectiveness of Medication-Assisted Treatment in Alcohol Use Disorder,” published in The Lancet (2020), MAT increased recovery success rates by 38%.
- Holistic Therapies: These approaches aim to treat the physical, emotional, and spiritual aspects of addiction using practices like meditation, yoga, acupuncture, and nutritional support. They enhance emotional resilience and promote healthier lifestyles. Holistic therapy complements clinical treatment by lowering stress and increasing body awareness. According to a study by Emily S. Walsh titled “Integrative Approaches to Alcohol Recovery,” published in the Journal of Alternative and Complementary Medicine (2019), holistic therapies reduced cravings and stress by 22%.
- Psychoeducation: Psychoeducation equips individuals with knowledge about addiction, treatment options, and relapse warning signs. It is delivered through lectures, reading materials, and interactive workshops. Educated patients are more likely to commit to treatment and sustain long-term recovery. According to a study by Deborah S. Finn titled “The Role of Psychoeducation in Alcohol Relapse Prevention,” published in Addiction Research & Theory (2021), psychoeducation reduced relapse rates by 29%.
What Kind of Alcohol Tests Does an Outpatient Rehab Use?
The kinds of alcohol tests an outpatient rehab uses are breathalyzer tests, urine ethyl glucuronide (EtG) tests, and blood tests. These tests help monitor recent alcohol use, ensure compliance with the recovery plan, and support accountability throughout structured treatment.
The kinds of alcohol tests an outpatient rehab uses are explained below:
- Breathalyzer tests: These tests measure blood alcohol content (BAC) through a handheld device that detects alcohol in a person’s breath. They provide immediate results and are often used before or after therapy sessions to verify sobriety. According to the National Highway Traffic Safety Administration (NHTSA), breathalyzers detect alcohol consumption within 12 hours of use.
- Urine Ethyl Glucuronide (EtG) tests: EtG tests detect alcohol metabolites in urine, offering a longer detection window—up to 80 hours after alcohol use. They are frequently used in outpatient settings for routine monitoring.
- Blood tests: Blood testing measures the exact blood alcohol content (BAC) and can identify alcohol presence with high accuracy shortly after consumption. These tests are typically used for medical evaluations or when immediate clinical verification is needed. According to a study by Daniel J. Lewis titled “Clinical Use of Blood Alcohol Testing in Outpatient Care,” published in American Journal of Clinical Pathology (2018), blood tests are considered the gold standard for precise BAC readings in time-sensitive situations.
How Much Does Outpatient Alcohol Rehab Cost in the U.S.?
Outpatient alcohol rehab costs in the U.S. range from $1,000 to $10,000 for a 30-day program. Factors influencing this cost include the program’s intensity, duration, location, and the specific services offered.
Standard outpatient programs are generally less expensive, while intensive outpatient programs (IOPs) and partial hospitalization programs (PHPs) incur higher fees due to increased therapy sessions and medical supervision. Additionally, amenities, staff qualifications, and facility reputation can further affect pricing.
What is the Average Cost of Outpatient Alcohol Rehab in North Carolina?
The average cost of outpatient alcohol rehab programs in North Carolina ranges between $5,000 and $10,000 for a 90-day program, averaging around $8,322. This amount is higher than the national average of $5,000 to $10,000 for a 30-day program.
This variation is influenced by factors such as program duration, intensity, and specific services offered. Additionally, facility amenities, staff qualifications, and geographic location contribute to cost differences between North Carolina and other states.
Is Outpatient Alcohol Rehab Covered by Insurance?
Yes, outpatient alcohol rehab is covered by insurance. Under the Affordable Care Act (ACA), substance use disorder services are classified as one of the ten essential health benefits, mandating that all Health Insurance Marketplace plans include coverage for these treatments.
Coverage specifics vary depending on the insurer and plan, but generally, private insurance, Medicaid, and Medicare offer some level of support for outpatient alcohol rehab services. Medicare, for instance, covers certain screenings and treatments related to alcohol misuse. It’s important to review your policy to understand the extent of coverage and any associated out-of-pocket costs.
What is the Success Rate of Outpatient Rehab in the U.S.?
The success rate of outpatient rehab in the U.S. is approximately 40% to 60% for individuals who complete treatment, depending on the program type and the level of engagement.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), 40% of people in outpatient alcohol rehab maintain long-term sobriety after treatment, with relapse being the most common challenge faced.
Key factors that improve outcomes include early intervention, the strength of the support system, ongoing therapy, and the integration of relapse prevention strategies. Studies by the National Institute on Alcohol Abuse and Alcoholism, 2020 show that individuals who engage in aftercare programs or continue therapy post-treatment have a 28% higher chance of sustaining sobriety.
How Does the Effectiveness of Outpatient Alcohol Rehab Compare to Inpatient Rehab?
The effectiveness of outpatient alcohol rehab compared to inpatient rehab is generally lower for individuals with severe alcohol use disorders, though both achieve similar outcomes for mild to moderate cases.
Inpatient rehab provides higher structure, 24/7 medical supervision, and full immersion in a recovery-focused environment, resulting in a success rate of up to 70% for individuals who complete treatment, according to a study by John F. Kelly titled “Treatment Outcomes in Alcohol Use Disorders” published in Alcohol Research: Current Reviews (2017). Outpatient rehab, while more flexible and cost-effective, shows a 40%–60% success rate, with a higher relapse risk due to continued exposure to external triggers and limited supervision.
The main differences lie in treatment intensity, accessibility, and relapse support—making inpatient rehab more effective for high-risk cases, while outpatient care suits those needing structured therapy without full residential commitment.
Who Are the Ideal Candidates for Outpatient Alcohol Rehab?
Individuals with mild to moderate alcohol use disorder (AUD), strong support systems, and stable home environments are ideal candidates for outpatient alcohol rehab. This level of care is best suited for those who are highly motivated, do not require 24/7 supervision, and maintain self-management while participating in structured therapy.
Outpatient rehab allows these individuals to continue work, school, or family obligations while actively engaging in their recovery process.
Is Outpatient Rehab Effective For People With Severe Alcoholism Withdrawal Symptoms?
No, outpatient rehab is not effective for people with severe alcoholism withdrawal symptoms. Severe withdrawal—including seizures, hallucinations, or delirium tremens—requires 24/7 medical supervision that outpatient programs cannot provide.
In such alcoholism withdrawal cases, inpatient rehab is necessary to ensure safety during detox and to manage potentially life-threatening complications, as outlined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Once stabilized, patients transition into outpatient care for continued structured therapy and relapse prevention.
Can Outpatient Alcohol Rehab Help With Co-occurring Mental Health Disorders?
Yes, outpatient alcohol rehab can help with co-occurring mental health disorders. Many programs offer dual diagnosis treatment, combining therapy sessions, psychiatric care, and medication management to address both alcohol use and conditions like depression, anxiety, or PTSD within a single mental health services.
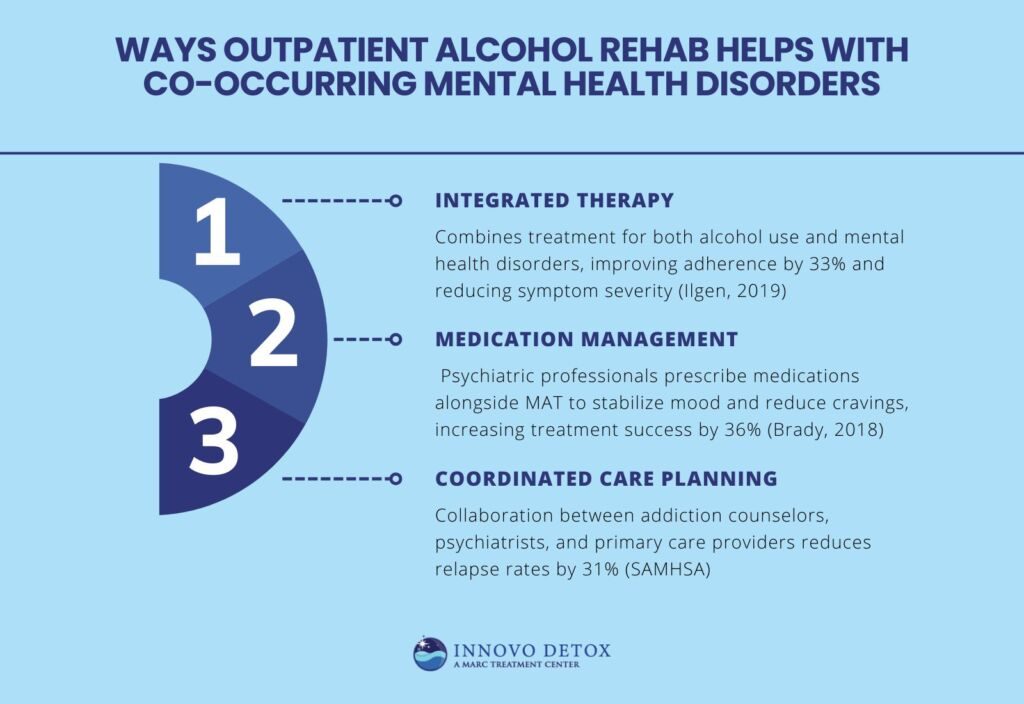
Ways outpatient alcohol rehab helps with co-occurring mental health disorders include:
- Integrated therapy: Outpatient programs treat dual diagnosis cases by offering coordinated care that addresses both alcohol use disorder and mental health conditions like depression or anxiety. Patients engage in individual therapy and group counseling tailored to both conditions. According to a study by Mark Ilgen titled “Treatment of Co-Occurring Disorders in Outpatient Care,” published in Journal of Dual Diagnosis (2019), integrated therapy improved treatment adherence by 33% and reduced symptom severity.
- Medication management: Psychiatric professionals in outpatient settings may prescribe antidepressants, anti-anxiety medications, or mood stabilizers alongside medication-assisted treatment (MAT) for alcohol use. This combined pharmacological approach helps stabilize mood while reducing cravings and withdrawal risk. A study by Kathleen Brady titled “Pharmacotherapy for Dual Diagnosis,” published in American Journal of Psychiatry (2018), found that combined medication protocols increased dual diagnosis treatment success rates by 36%.
- Coordinated care planning: Dual diagnosis programs in outpatient rehab involve collaboration between addiction counselors, psychiatrists, and primary care providers. This ensures a unified recovery plan with consistent communication and progress tracking. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), coordinated outpatient care reduced relapse rates by 31% in patients with co-occurring conditions.
What Are the Signs that Outpatient Alcohol Rehab May Not Be Enough for Recovery?
The signs that outpatient alcohol rehab may not be enough for recovery include frequent relapse, inability to maintain sobriety outside of sessions, and severe withdrawal symptoms.
These alcohol relapse indicators suggest the need for more intensive care, such as inpatient rehab, where 24/7 medical supervision and structured support provide the necessary stability for sustained alcohol recovery.
The signs that outpatient alcohol rehab may not be enough for recovery are explained below:
- Frequent relapses: Repeated returns to alcohol use after completing sessions suggest that outpatient care alone may lack the structure needed. This pattern often indicates unresolved triggers or insufficient support. According to the National Institute on Drug Abuse (NIDA), 40% to 60% of individuals in outpatient rehab experience relapse, which require transitioning to inpatient care.
- Inability to maintain sobriety between sessions: When individuals struggle to stay sober outside of therapy sessions, even for short periods, it shows the need for a more immersive environment. Inpatient rehab offers constant monitoring and zero-access settings that prevent use.
- Lack of family or social support: Outpatient rehab depends on a stable and supportive home life. If the person lives in a triggering or unsupportive environment, progress are undermined. Without a solid support system, outpatient care are not be sustainable.
- Severe mental health issues: Co-occurring disorders like bipolar disorder, PTSD, or major depression that interfere with daily functioning require intensive psychiatric support. Outpatient programs do not provide the depth of care or medication oversight needed. In such cases, dual diagnosis treatment in a residential setting is more appropriate.
How to Choose the Right Outpatient Alcohol Rehab?
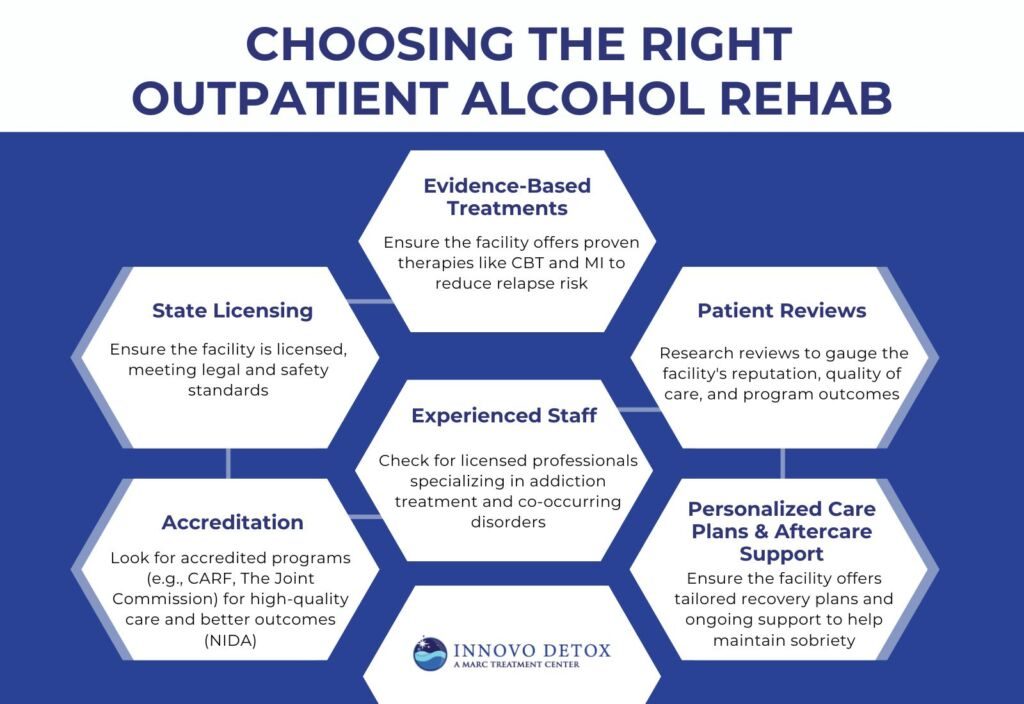
To choose the right outpatient alcohol rehab, consider factors like program specialization, therapy options, and staff qualifications. It’s important to select a facility that offers tailored recovery plans and has experience handling co-occurring disorders or specific needs, such as trauma or family therapy.
Tips to choose the right outpatient alcohol rehab are explained below:
- State licensing: Ensure the facility is licensed by the state to provide substance use treatment. This confirms that the program meets legal and safety standards and adheres to regulations regarding patient care. Licensing ensures that the facility is regularly inspected for quality and compliance with industry standards.
- Accreditation: Look for accredited programs from reputable organizations such as CARF (Commission on Accreditation of Rehabilitation Facilities) or The Joint Commission. Accreditation signifies that the program meets or exceeds national treatment standards and provides high-quality care. According to the National Institute on Drug Abuse (NIDA), accredited facilities have consistently better patient outcomes.
- Evidence-based treatments: The facility should offer evidence-based treatments, such as cognitive-behavioral therapy (CBT) and motivational interviewing (MI), which have proven effective in treating alcohol use disorder. These therapies help address the root causes of addiction and reduce the risk of relapse.
- Experienced staff: Ensure that the facility employs licensed and experienced professionals, including counselors, therapists, and medical staff, who specialize in addiction treatment. Staff with expertise in both alcohol use disorder and co-occurring mental health conditions provide the best chance for long-term recovery.
- Patient reviews: Research patient reviews and testimonials to gauge the facility’s reputation. Positive feedback indicates the quality of care, staff support, and program outcomes, while negative reviews can help highlight potential issues. Facilities with strong, consistent patient satisfaction scores are more likely to offer a personalized care plan that supports individual recovery needs.
- Personalized care plans and aftercare support: A good outpatient facility will develop a personalized care plan tailored to the individual’s unique needs and goals. Aftercare support is equally important, providing resources such as ongoing therapy, support groups, or relapse prevention programs. This continuous support helps prevent relapse and fosters long-term recovery.
What Qualifications Should You Look for in an Outpatient Alcohol Rehab Facility?
The qualifications to look for in an outpatient alcohol rehab facility are state licensing, accreditation from reputable organizations like CARF or The Joint Commission, and the availability of evidence-based treatments. Additionally, ensure the facility employs experienced staff, offers personalized care plans, and provides aftercare support to ensure long-term recovery.
The qualifications you should look for in an outpatient alcohol rehab facility include the following:
- Accreditation from CARF (Commission on Accreditation of Rehabilitation Facilities): CARF accreditation signifies that the rehab facility meets rigorous standards for quality and patient care. CARF-accredited facilities are committed to improving patient outcomes and maintaining a high standard of service across various treatment modalities.
Accreditation from The Joint Commission: The Joint Commission’s accreditation ensures that the rehab facility complies with the highest healthcare standards for patient care and safety. Facilities with this accreditation demonstrate their dedication to ongoing quality improvement and effective treatment outcomes, following evidence-based practices.