Alcohol addiction develops in stages. In the early stage, you may drink to relieve stress, build a tolerance, and deny there’s a problem, needing more alcohol over time to feel the same effects.
The middle stage signals growing dependence. You may find it harder to control how much you drink, feel strong cravings, and start pulling away from responsibilities or relationships. According to the National Centre for Drug Abuse Statistics (NCDAS), 18.5% of Pennsylvania adults over the age of 18 engage in binge drinking at least once per month.
In the late stage, drinking becomes compulsive. Health issues worsen, thinking becomes clouded, and control over alcohol use fades completely.
Treatment depends on where you are. Early-stage care includes therapy or outpatient support. Middle-stage addiction usually needs detox and medication. For late-stage, inpatient rehab and long-term therapy provide the structure needed for recovery.
What Is the Early Stage of Alcohol Addiction?
The early stage of alcohol addiction starts quietly — a shift from occasional or social drinking to using alcohol more regularly. You might begin turning to alcohol to manage stress, emotions, or uncomfortable social situations.
At this point, psychological dependence begins to take hold. You’re not dealing with physical withdrawal yet, but drinking becomes less about fun and more about coping. What once happened only at gatherings starts happening alone, and more. You start to rely on alcohol to feel okay, and that’s when the pattern begins to take root.
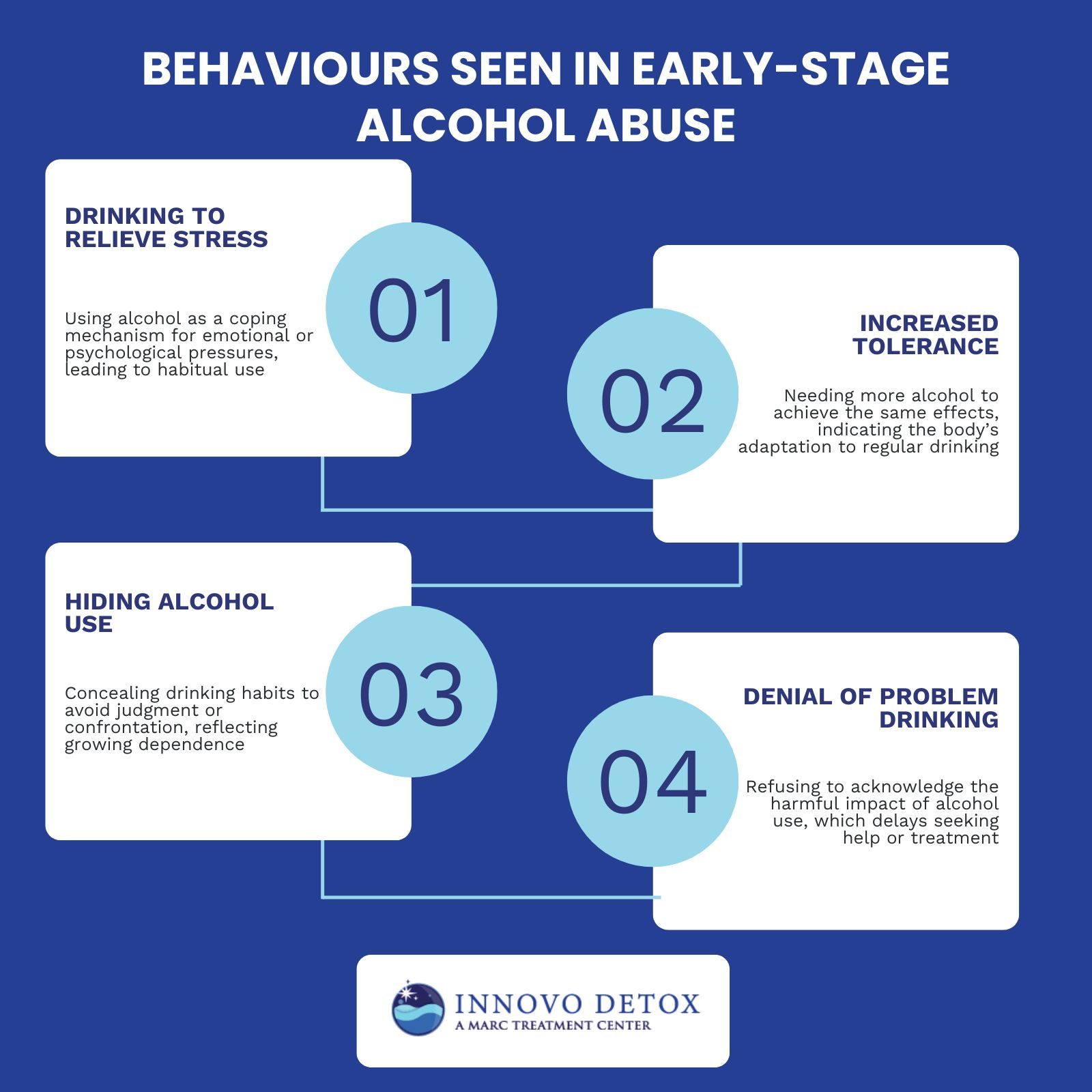
What Behaviours Show Early-Stage Alcohol Abuse?
The behaviours that show at the early stage of alcohol abuse include drinking to relieve stress, increased tolerance, hiding alcohol use, and denial of problem drinking. In the early stage of alcohol addiction, the signs are easy to overlook, especially when you’re using alcohol to cope.
The behaviors that show early-stage alcohol abuse are explained below:
Drinking to Relieve Stress
You might start turning to alcohol when you’re overwhelmed, after a long day, during arguments, or when anxious. It feels like a quick fix. Over time, this habit builds into a routine where alcohol becomes your go-to way of coping, not just a drink.
Increased Tolerance
You notice one or two drinks don’t affect you the way they used to. So, you drink more. Your body adjusts, and now you need larger amounts to feel the same effect. That creeping tolerance is a warning sign — your system is adapting in a way that pulls you deeper into addiction.
Hiding Alcohol Use
As your drinking becomes more frequent, you start drinking in private or making excuses to avoid being noticed. You don’t want questions or judgment, so you hide it, but that secrecy shows that alcohol is beginning to take control.
Denial of Problem Drinking
Even if others raise concerns, you brush them off. “I’m just stressed,” or “I only drink on weekends.” These justifications are common in early addiction. Denial keeps you from seeing the impact, and delays the chance to get help before things get worse.
Recognising these behaviours early makes all the difference. The sooner you face them, the easier it becomes to break the pattern and take back control.
What Is The Middle Stage of Alcohol Addiction?
In the middle stage of alcohol addiction, drinking shifts from habit to dependence. You feel intense cravings and experience withdrawal symptoms when you try to stop — your body and mind have started relying on alcohol to function.
At this point, your tolerance has grown even more. It takes larger amounts to feel the same relief or escape, and alcohol becomes your main way of coping with stress or anxiety.
As the addiction deepens, everyday life begins to slip. You start neglecting work, relationships, or your health, but you keep drinking anyway, even when you see the damage it’s causing. This stage shows just how deeply alcohol has taken hold.
What Are the Warning Signs of Middle-Stage Alcoholism?
The warning signs for middle-stage alcoholism include increased drinking despite negative consequences, physical withdrawal symptoms, hiding alcohol use, and neglecting responsibilities. As alcohol dependence deepens, individuals find themselves unable to reduce consumption, even when faced with serious consequences.
The warning signs of middle-stage alcoholism are explained below:
Increased Drinking Despite Negative Consequences
Individuals continue to increase their alcohol consumption, even when negative consequences, such as deteriorating relationships or health issues, arise. This behaviour is driven by the individual’s inability to control their drinking due to the growing psychological and physical dependence on alcohol.
Physical Withdrawal Symptoms
The central nervous system, which has become reliant on alcohol’s depressant effects, becomes hyperactive, leading to symptoms like tremors, sweating, nausea, and anxiety. These symptoms signify a shift from moderate to severe dependence, requiring medical intervention to safely manage the withdrawal process and prevent complications such as seizures.
Hiding Alcohol Use
Individuals begin to drink in secrecy, concealing their drinking habits from friends, family, and colleagues to avoid judgment or confrontation. This behaviour arises as alcohol consumption escalates, and the individual feels a growing need to drink despite its negative effects on their personal and professional life.
Neglecting responsibilities
As alcohol use intensifies, individuals begin to prioritise drinking over work, relationships, and other obligations. This neglect reflects how alcohol addiction starts to dominate their daily life, impairing their ability to meet personal and professional responsibilities.
What Is The Late Stage Of Alcohol Addiction?
The late stage of alcohol addiction, also known as end-stage alcoholism, is marked by severe physical and psychological consequences. At this point, alcohol use has led to irreversible damage to vital organs such as the liver, heart, and brain. Chronic alcohol abuse results in liver diseases like cirrhosis, heart complications, and cognitive decline.
Individuals in the late stage of alcohol addiction face life-threatening health issues, including memory loss, impaired motor skills, and an inability to function without alcohol.
The body’s ability to tolerate alcohol diminishes, and withdrawal symptoms become more intense. Cognitive impairment and emotional instability are common, making it difficult for individuals to maintain relationships or manage daily activities.
What Are Signs And Symptoms Of Late-Stage Alcoholism?
The signs and symptoms of late-stage alcoholism include liver disease (cirrhosis), memory loss and cognitive impairment, severe withdrawal symptoms, and a loss of control over drinking. As the addiction progresses, individuals experience irreversible damage to vital organs.
The signs and symptoms of late-stage alcoholism are explained below:
Liver Disease (Cirrhosis)
Liver disease, specifically cirrhosis, is one of the most severe consequences of long-term alcohol abuse. Cirrhosis occurs when the liver becomes severely scarred due to the prolonged inflammation caused by alcohol’s toxic effects. Over time, this scarring disrupts the liver’s ability to function, leading to liver failure and other complications.
According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), approximately 10-20% of heavy drinkers develop cirrhosis after years of alcohol consumption.
Memory Loss and Cognitive Impairment
Memory loss and cognitive impairment are common consequences of long-term alcohol abuse. Chronic alcohol consumption leads to changes in the brain, affecting memory, learning, and cognitive function. This occurs because alcohol interferes with neurotransmitter systems, leading to a reduction in brain cell function and damage over time.
Severe Withdrawal Symptoms
Symptoms such as tremors, anxiety, seizures, and delirium tremens (DTs) are common in severe cases. Delirium tremens is a particularly dangerous condition that includes confusion, agitation, and hallucinations, and it is fatal without proper medical intervention.
Loss of control over drinking
Loss of control over drinking is a critical symptom of late-stage alcoholism, where the individual no longer regulates alcohol consumption despite the clear negative consequences on their health, relationships, and daily functioning. At this stage, individuals attempt to quit or reduce their drinking but find themselves unable to stop or limit their intake.
What Are the Effects of Alcoholism?
The effects of alcoholism include liver and heart disease, mental health disorders, job loss and financial instability, relationship breakdown, cardiovascular issues, digestive problems, Wernicke-Korsakoff syndrome, and mental health decline. Alcohol addiction disrupts various facets of life, leading to an increased risk of death.
The effects of alcoholism are explained below:
- Liver and Heart Disease: Chronic alcohol consumption leads to liver damage, including cirrhosis, which hinders liver function. Over time, alcohol strains the heart, increasing the risk of heart disease and high blood pressure.
- Mental Health Disorders: Alcoholism affects mental health, contributing to conditions like anxiety and depression. These disorders worsen over time, as alcohol alters brain chemistry and impairs the individual’s ability to regulate mood.
- Job Loss and Financial Instability: Alcoholism negatively impacts work performance, leading to missed days, decreased productivity, and ultimately, job loss.
- Relationship Breakdown: Alcoholism is a leading cause of relationship issues, including divorce and family estrangement. The emotional and physical toll alcohol takes on both the drinker and their loved ones contributes to conflict.
- Cardiovascular Issues: Alcohol increases the risk of cardiovascular problems such as high blood pressure and arrhythmias. Chronic drinking weakens the heart muscles, potentially leading to heart failure.
- Digestive Problems: Alcohol severely impacts the digestive system, causing issues like gastritis, ulcers, and pancreatitis. Alcohol’s irritating effect on the stomach lining leads to inflammation and digestive discomfort.
- Wernicke-Korsakoff Syndrome: This syndrome is a brain disorder linked to long-term alcohol abuse and thiamine deficiency. It results in memory problems, confusion, and issues with motor coordination. If untreated, Wernicke-Korsakoff syndrome causes permanent brain damage and cognitive decline.
- Mental Health Decline: Chronic alcohol abuse contributes to cognitive impairments, including memory loss and reduced decision-making abilities. Alcohol-related brain damage affects the individual’s ability to think clearly and process information.
- Immune System Suppression: Long-term alcohol abuse weakens the immune system, making individuals more susceptible to infections. Alcohol impairs the body’s ability to fight off illnesses, increasing the risk of chronic diseases like tuberculosis and pneumonia.
- Risk of Death: Chronic alcoholism increases the risk of premature death due to complications such as liver failure, heart disease, and alcohol poisoning. Accidental injuries, such as falls and traffic accidents, are also common among individuals with alcohol addiction.
What Are the Risk Factors for Alcohol Addiction?
The risk factors of alcohol addiction include steady drinking, early age drinking, bariatric surgery, a history of trauma, and other environmental and genetic factors. Steady drinking increases the likelihood of alcohol dependence, as regular consumption leads to physical and psychological adaptation to alcohol. Drinking at an early age, especially during adolescence, disrupts brain development and increases the risk of addiction later in life.
Having bariatric surgery raises the risk of alcohol addiction due to changes in how the body absorbs alcohol, resulting in faster intoxication and potentially greater consumption. A history of trauma, including physical or emotional abuse, drives individuals to use alcohol as a coping mechanism, making them more susceptible to addiction.
Other contributing factors include genetic predispositions, mental health conditions, and environmental influences, all of which heighten the risk of alcohol dependency.
How Is Alcohol Addiction Diagnosed?
Alcohol addiction is diagnosed through a combination of clinical evaluations, diagnostic criteria, and screening tests. The DSM-5 provides guidelines for diagnosing alcohol use disorder (AUD), which include a pattern of alcohol use leading to impairment or distress.
A doctor assesses the severity of symptoms based on criteria such as increased tolerance, unsuccessful attempts to cut down, and withdrawal symptoms.
Screening tests like the AUDIT (Alcohol Use Disorders Identification Test) are widely used to identify problematic drinking patterns and determine the level of risk.
How Is AUD Severity Classified?
AUD severity is classified into three levels: mild, moderate, and severe. Each level reflects the severity of symptoms and the degree of impact alcohol use has on a person’s life.
Aud severity classification is explained below:
- Mild: Mild AUD involves the presence of 2 to 3 criteria from the DSM-5. Individuals at this level show some signs of alcohol-related issues, but the consequences are less severe. Intervention at this stage involves outpatient therapy and lifestyle changes.
- Moderate: Moderate AUD includes 4 to 5 criteria from the DSM-5. At this stage, individuals experience more disruptions in their daily lives due to alcohol use. Treatment requires a combination of outpatient care, counselling, and sometimes medication-assisted therapy.
- Severe: Severe AUD is characterised by six or more criteria from the DSM-5. Individuals at this level face major health, social, and psychological issues caused by alcohol abuse. Intensive treatment, including inpatient care, medical supervision, and long-term therapy, is usually necessary.
What Are The Treatment Options For Alcohol Addiction?
The treatment options for alcohol addiction are detoxification, medication-assisted treatment, behavioural therapy, and support groups. Alcohol addiction treatment involves a comprehensive approach that addresses specific facets of alcohol use disorder, from managing withdrawal symptoms to fostering long-term recovery.
The treatment options for alcohol addiction include the following:
Detoxification
Detoxification is the first step in the treatment of alcohol addiction. It involves safely removing alcohol from the body while managing withdrawal symptoms. This process is important to stabilise the individual physically before further treatment, such as therapy or medication, is introduced.
During detox, the body rids itself of alcohol, which leads to withdrawal symptoms like anxiety, tremors, and seizures. Medical supervision is necessary to ensure the individual’s safety, especially in cases of severe alcohol dependence.
Medication-Assisted Treatment
Medication-Assisted Treatment (MAT) is an approach to alcohol addiction recovery that combines the use of medications with counselling and therapy. The goal of MAT is to reduce cravings, prevent relapse, and promote long-term recovery. Medications like disulfiram, naltrexone, and acamprosate are commonly prescribed to help individuals manage alcohol dependence and maintain sobriety.
Behavioural Therapy
Behavioural Therapy is an important component of alcohol addiction treatment. It focuses on changing harmful drinking behaviours and developing coping strategies to manage triggers and stressors that lead to relapse. Cognitive Behavioural Therapy (CBT) and Motivational Interviewing (MI) are two common forms of therapy used in alcohol addiction treatment.
Support Groups
Support Groups are an important part of alcohol addiction treatment, providing individuals with a community of peers who share similar experiences and challenges. These groups, such as Alcoholics Anonymous (AA) and SMART Recovery, offer a supportive environment where individuals share their struggles, receive encouragement, and learn strategies for maintaining sobriety.
Can I Use Insurance for Alcohol Addiction Treatment in Ohio?
Yes, you can use insurance to cover alcohol addiction treatment in Ohio. Thanks to federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA), most health insurance plans are required to cover substance use disorder treatments, including those for alcohol addiction. This coverage includes detoxification, inpatient and outpatient rehabilitation, therapy, and medication-assisted treatment.