Oxycodone addiction is a growing concern in the US, reflecting the misuse of one of the most commonly prescribed painkillers, Oxycodone. Initially intended to alleviate moderate to severe pain, oxycodone’s powerful effects on the brain’s reward system lead to dependency and compulsive use. This condition disrupts daily life and poses serious health risks, requiring immediate attention and professional intervention.
According to the CDC, opioids, including oxycodone, accounted for nearly 75% of all drug overdose deaths in the U.S. in 2021. Worldwide, the opioid epidemic has reached alarming levels, with millions of individuals misusing prescribed painkillers such as oxycodone, hydrocodone, and codeine, underscoring the urgent need for preventive measures and effective treatments.
The primary causes of oxycodone addiction include prolonged use, misuse of prescriptions, and genetic predisposition to substance abuse. Emotional stress, chronic pain, and easy access to opioids further exacerbate the risk. A study by CAMH titled “Mental Illness and Addiction” also reveals that individuals with a history of mental health disorders or trauma are significantly more susceptible to developing a dependency on oxycodone.
The signs and symptoms of oxycodone addiction are both physical and behavioral. Common indicators include increased tolerance, withdrawal symptoms, compulsive drug-seeking behavior, and noticeable changes in mood or daily habits. These warning signs escalate over time, making early detection important for effective intervention.
The effects of oxycodone addiction extend beyond physical health, impacting mental well-being, relationships, and financial stability. Prolonged misuse leads to liver damage, respiratory issues, and overdose risks while also straining personal and professional relationships. The societal toll, including lost productivity and healthcare costs, further highlights the devastating impact of this addiction.
Effective treatment options for oxycodone addiction include medical detoxification, medication-assisted treatment (MAT), behavioral therapies, and support groups. Programs customized to individual needs have shown significant success in managing withdrawal symptoms, reducing cravings, and addressing the root causes of addiction. Seeking professional help for Oxycodone addiction is important for achieving long-term recovery and rebuilding a healthier, more fulfilling life.
What Is Oxycodone Addiction?
Oxycodone addiction is a physical and psychological dependence on the drug, leading to compulsive use despite harmful consequences. As a semi-synthetic opioid prescribed for moderate to severe pain, oxycodone produces euphoria, increasing the risk of misuse and addiction.
Oxy addiction is a significant component of the broader opioid crisis in the United States. Opioids, including prescription medications like oxycodone, are highly addictive and have been major contributors to the drug overdose epidemic. The National Institute on Drug Abuse (NIDA) reports that the vast majority of overdose deaths in recent years involved illicitly manufactured fentanyl and other potent synthetic opioids.
In Pennsylvania, the impact of oxycodone addiction is profound. According to the Pennsylvania Office of Attorney General, in 2021, 5,168 Pennsylvanians died from opioid overdoses, averaging 14 deaths per day. This alarming statistic emphasizes the severity of the opioid epidemic within the state.
What Is Oxycodone and How Is It Used?
Oxycodone is a prescription opioid medication used primarily for pain relief and pain management. It works by binding to opioid receptors in the brain and spinal cord to reduce pain perception. Common brand names for oxycodone include OxyContin, Percocet (when combined with acetaminophen), and Roxicodone.
Medically, oxycodone is prescribed for moderate to severe pain for conditions such as post-surgical recovery, cancer-related pain, or chronic pain management. It is available in various forms, including immediate-release tablets, extended-release formulations, and liquid solutions. While effective for pain relief, oxycodone carries a significant potential for misuse due to its euphoric effects, leading to dependency in some patients.
The potential for misuse arises from oxycodone’s ability to induce feelings of euphoria when taken in high doses or through methods not prescribed, such as crushing and snorting tablets. This risk is compounded by its high bioavailability and rapid onset of effects, making it one of the most commonly misused prescription opioids.
Why Is Oxycodone So Addictive?
Oxycodone is highly addictive because it interacts directly with brain receptors, specifically the mu-opioid receptors, to produce pain relief and intense feelings of euphoria. This pleasurable sensation reinforces the behavior of taking the drug, creating a cycle of reward and craving. Over time, the brain’s natural ability to produce dopamine is diminished, leading to dependence on the drug for normal functioning.
A study by Kosten TR, George TP. et al. 2002, titled “The neurobiology of opioid dependence: implications for treatment,” has shown that repeated oxycodone use alters the brain’s reward pathways, making it increasingly difficult to experience pleasure from natural stimuli. According to the National Institute on Drug Abuse (NIDA), opioid addiction mechanisms are deeply rooted in these neurochemical changes, which foster both physical dependence and compulsive drug-seeking behavior.
How Does Oxycodone Addiction Develop?
Oxycodone addiction develops in stages, starting with legitimate prescription use. In this initial stage, patients use the medication as directed for pain management. Over time, tolerance develops, requiring higher doses to achieve the same level of pain relief.
The second stage involves misuse, where the individual begins taking oxycodone in ways not prescribed, such as increasing the dose or using it for euphoric effects. This stage is marked by a psychological attachment to the drug’s effects.
In the final stage, dependence and addiction occur. Physical dependence is characterized by withdrawal symptoms when the drug is not taken, while addiction involves compulsive use despite negative consequences. Escalation of use follows as individuals require increasing amounts to overcome tolerance and avoid withdrawal symptoms.
How Long Does It Take to Get Addicted to Oxycodone?
It takes a few weeks to get addicted to oxycodone, but this timeline varies based on individual factors, including dosage, frequency of use, and personal susceptibility. A clinical study by Psychiatry.org suggests that dependence develops within 4 to 8 weeks of regular use, especially at high doses. For some individuals, misuse or addiction occurs within days if the drug is taken in ways not prescribed, emphasizing the importance of careful medical supervision.
What Causes Oxycodone Addiction?
The causes of oxycodone addiction include a combination of biological, psychological, and social factors that interact to increase vulnerability to dependency. Addiction stems from the drug’s potent effects on the brain’s reward system, making users reliant on its euphoric and pain-relieving properties. Environmental influences, such as access to prescriptions and social pressures, further increase vulnerability to misuse and dependency.
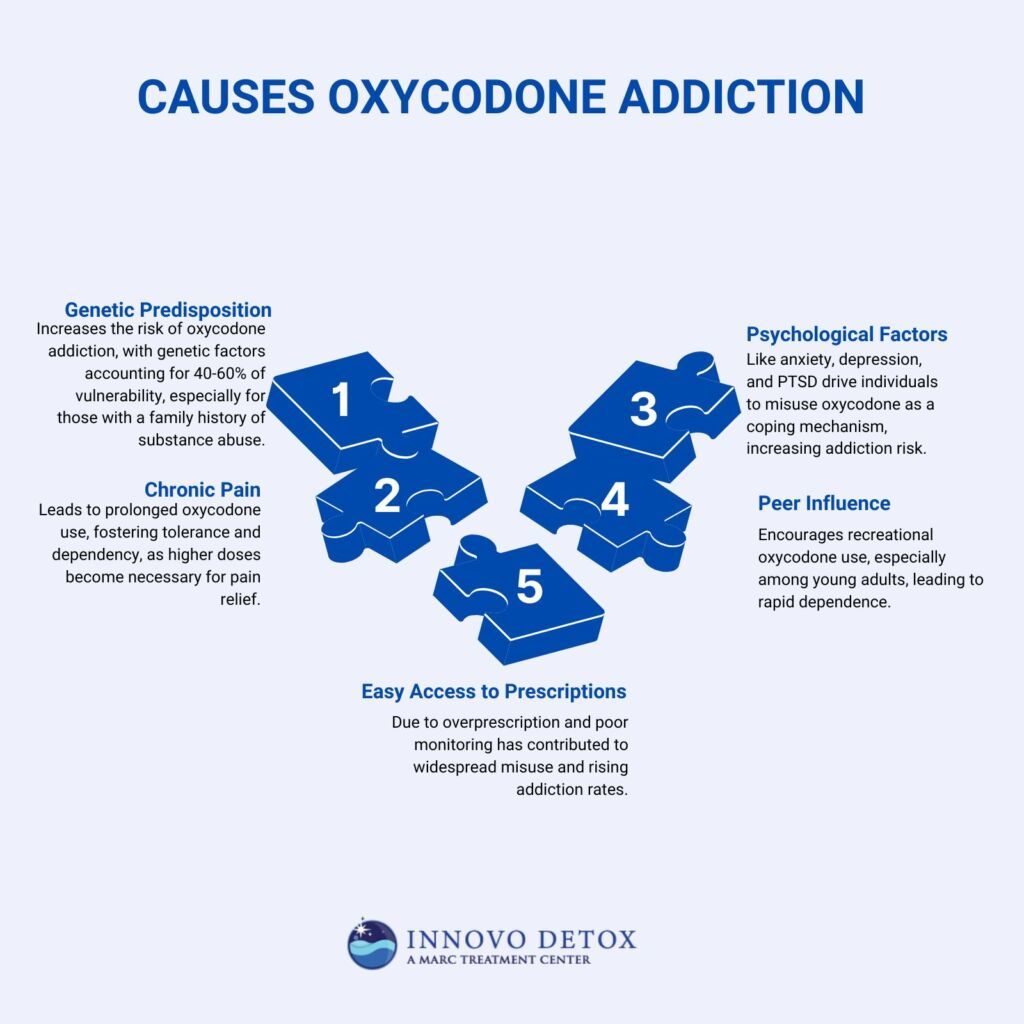
These causes of oxycodone addiction are described as follows:
- Genetic Predisposition: Genetic predisposition refers to an individual’s inherited likelihood of developing addiction due to variations in genes affecting brain chemistry and dopamine regulation. A neurobiological study by Prescott CA, Kendler KS. et al. 1999, titled “Genetic and environmental contributions to alcohol abuse and dependence in a population-based sample of male twins,” indicates that genetic factors account for 40-60% of a person’s vulnerability to addiction. Individuals with a family history of substance abuse are more likely to develop oxycodone addiction due to inherited differences in brain chemistry that affect dopamine regulation.
- Chronic Pain: Chronic pain conditions lead to long-term oxycodone prescriptions, increasing the risk of dependence. According to a study by Chou R et al. 2015, titled “The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention workshop,” prolonged use for pain management results in tolerance, where higher doses are needed to achieve the same relief, fostering a cycle of misuse.
- Psychological Factors: Conditions such as anxiety, depression, and post-traumatic stress disorder (PTSD) are strongly associated with a higher risk of opioid addiction. According to a study by the National Center for PTSD titled “Opioid Use Among Individuals with Posttraumatic Stress Disorder,” PTSD impacts 1 in 5 Americans, and these individuals misuse opioids like oxycodone as a coping mechanism to alleviate emotional distress.
- Peer Influence: Social environments play a significant role in initiating misuse. Adolescents and young adults, in particular, begin using oxycodone recreationally due to peer pressure, which quickly escalates into addiction.
- Easy Access to Prescriptions: Overprescription of oxycodone and lack of stringent monitoring have contributed to widespread availability, making it easier for individuals to misuse the drug. States with high prescription rates, such as Pennsylvania, have seen corresponding spikes in addiction rates. At least 2 million people have an opioid use disorder (OUD) involving prescription opioids, and almost 600,000 have an OUD associated with heroin, as studied by the Substance Abuse and Mental Health Services Administration (SAMHSA).
What Are the Risk Factors for Oxycodone Addiction?
The risk factors for Oxycodone addiction are family history of addiction, chronic pain, mental health issues, access to prescriptions, and certain demographic characteristics. Individuals with a family history of substance abuse and those with chronic pain are prescribed oxycodone, which increases the risk of misuse and dependency. People with mental health disorders like depression or anxiety use oxycodone as a form of self-medication, raising their vulnerability to addiction. Age, especially younger individuals or those with a history of substance abuse, further increases the likelihood of becoming addicted.
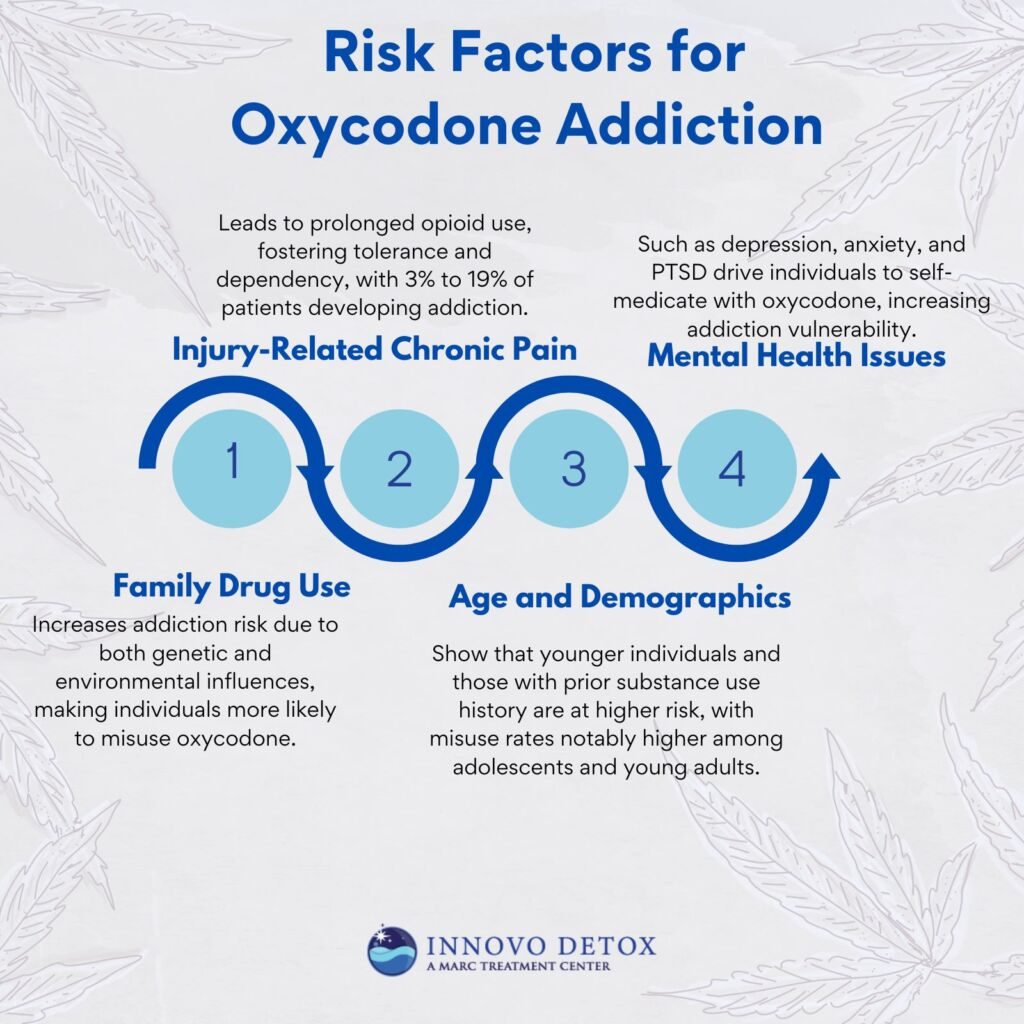
The risk factors for Oxycodone addiction are as follows:
- Family using drugs: Individuals who grow up in households where drug use is prevalent have a higher risk of developing addiction themselves. According to a Mayo Clinic study titled “How Opioid Use Disorder Occurs,” those with family members struggling with substance abuse are more likely to develop a dependency on prescription opioids like oxycodone due to both genetic and environmental influences.
- Injury-causing chronic pain: Severe injuries requiring long-term opioid pain management put individuals at a higher risk of developing oxycodone addiction. As the body builds tolerance, higher doses are needed for relief, increasing dependency. According to the American Medical Association (AMA), 3% to 19% of those prescribed opioids for injury pain develop an addiction.
- Mental health issues: Those with mental health disorders such as depression, anxiety, or PTSD are more vulnerable to using oxycodone as a form of self-medication, raising their risk of developing an addiction. Over 60 percent of adolescents in community-based substance use disorder treatment programs also meet diagnostic criteria for another mental illness, as studied by Hser YI, Grella CE, Hubbard RL, et al. 2001, titled “An evaluation of drug treatments for adolescents in 4 US cities.”
- Age and demographics: Younger individuals and those with a history of prior substance abuse are particularly at risk. In 2016, 3.6% of adolescents ages 12 to 17 years and 7.3% of emerging adults ages 18 to 25 years misused an opioid in the United States, according to the 2016 National Survey on Drug Use and Health.
What Role Does Trauma Play in Oxycodone Addiction?
Trauma plays a significant role in Oxycodone addiction by increasing the likelihood of individuals turning to opioids as a form of self-medication. Past trauma, such as abuse or PTSD, leads to emotional and psychological distress, which individuals attempt to numb using oxycodone. The emotional triggers linked to traumatic experiences drive people to misuse opioids to cope with feelings of anxiety, fear, or depression. A study by Flanagan JC, Korte KJ, Killeen TK, Back SE. et al. 2016, titled “Concurrent Treatment of Substance Use and PTSD, has shown that individuals with PTSD are at a higher risk of developing opioid addiction, with study findings indicating that up to 30% of people with PTSD also suffer from substance use disorders, including oxycodone dependence.
What Are the Signs and Symptoms of Oxycodone Addiction?
The signs and symptoms of Oxycodone addiction are physical, behavioral, and emotional, and each varies in intensity depending on the severity of the addiction. These symptoms are a result of how oxycodone interacts with the brain and body, altering neurotransmitter systems and affecting cognitive and physical functioning.
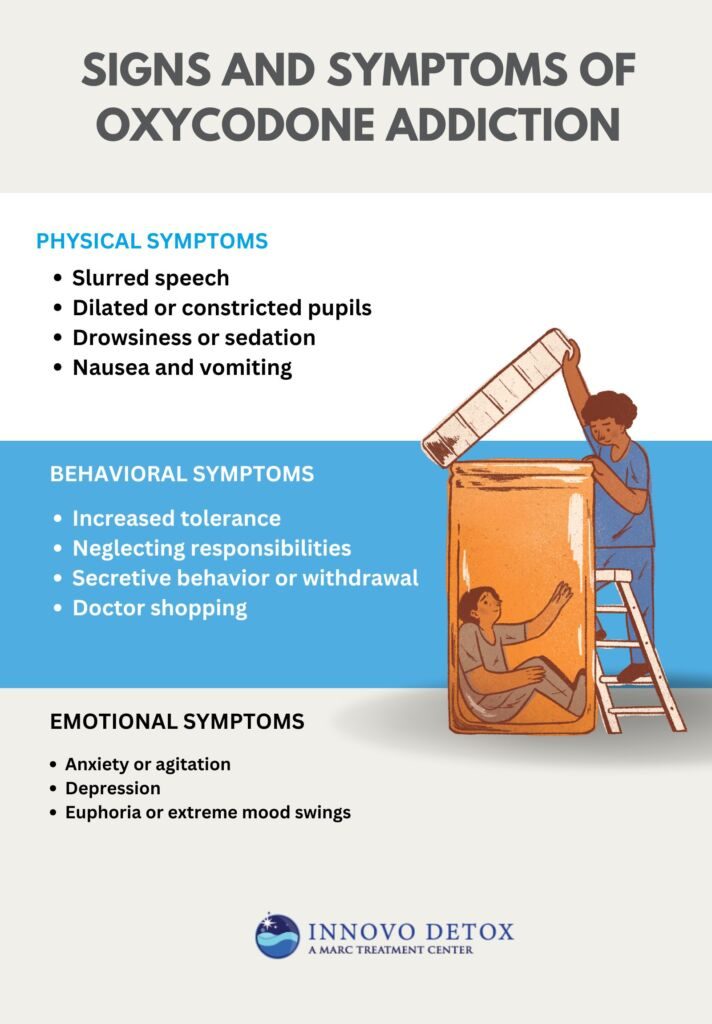
The physical signs and symptoms of Oxycodone addiction are as follows:
- Slurred speech: Slurred speech is a primary symptom of opioid use, including oxycodone. This occurs because oxycodone depresses the central nervous system, impairing muscle control and the coordination required for speech. This symptom is mild in early addiction stages but becomes more pronounced as dependency deepens. A study from the National Institute on Drug Abuse (NIDA) found that 60% of individuals with opioid use disorder exhibit physical signs of motor impairment, including slurred speech.
- Dilated or constricted pupils: Oxycodone and other opioids cause constriction of the pupils, a phenomenon known as miosis. This happens because opioids bind to receptors in the brain, specifically in the brainstem, which controls pupil size. Constricted pupils are a common physical sign of opioid intoxication. Research by Trescot AM et al. 2008, titled “Opioid Pharmacology,” shows that over 90% of people using opioids, including oxycodone, exhibit this symptom during active use or intoxication.
- Drowsiness or sedation: Sedation is one of the most common and severe physical symptoms of oxycodone addiction. The drug depresses the central nervous system, leading to extreme drowsiness, lethargy, and a reduced ability to stay awake. This sedative effect becomes dangerous, leading to confusion, inability to perform basic tasks, and even accidental overdose. A clinical study by the Centers for Disease Control and Prevention (CDC), titled “CDC Guideline for Prescribing Opioids for Chronic Pain,” indicates that oxycodone users experience significant drowsiness, with the severity increasing with prolonged use.
- Nausea and vomiting: Nausea and vomiting are common symptoms, especially during the early stages of addiction or withdrawal. Oxycodone interferes with the gastrointestinal system by slowing down digestion and increasing sensitivity to certain stimuli. According to a study by Camilleri M, Lembo A, Katzka DA. et al. 2017, titled “Opioids in Gastroenterology: Treating Adverse Effects and Creating Therapeutic Benefits,” show that individuals abusing opioids report gastrointestinal distress, including nausea and vomiting, which worsens during withdrawal phases.
The behavioral signs and symptoms of Oxycodone addiction are as follows:
- Increased tolerance: Tolerance refers to the need to take progressively higher doses of oxycodone to achieve the same effects. This happens because the brain and body adjust to the presence of the drug, requiring more to produce the desired response. Over time, this leads to escalating doses, increasing the risk of overdose. A study by Darnall BD, Stacey BR, Chou R., et al. 2012, titled “Medical and psychological risks and consequences of long-term opioid therapy in women,” indicates that long-term oxycodone users experience increased tolerance, which is a major driver of addiction.
- Neglecting responsibilities: As addiction takes hold, individuals neglect work, school, or social responsibilities. This is because the brain’s reward system, which is hijacked by oxycodone, prioritizes drug use over other activities. Individuals addicted to prescription opioids report neglecting their personal and professional duties due to their obsession with obtaining and using the drug.
- Secretive behavior or withdrawal: People with oxycodone addiction become secretive about their drug use. They go to great lengths to hide their addiction from family and friends, including lying about their whereabouts or avoiding social situations. This is driven by feelings of shame, guilt, and the fear of being caught. Withdrawal symptoms, such as anxiety and agitation, also make it difficult for individuals to maintain normal relationships. A study by the Substance Abuse and Mental Health Services Administration (SAMHSA) found that about 50% of individuals who misuse prescription opioids engage in secretive behavior to hide their addiction.
- Doctor shopping: Doctor shopping is a common behavioral symptom where individuals visit multiple healthcare providers to obtain prescriptions for oxycodone without informing each doctor about the others. This is done to maintain a continuous supply of the drug. Research by Simeone R et al. 2017 titled “Doctor Shopping Behavior and the Diversion of Prescription Opioids” shows that up to 30% of individuals with opioid use disorder engage in doctor shopping as part of their addiction cycle.
The emotional signs and symptoms of Oxycodone addiction are as follows:
- Anxiety or agitation: Anxiety and agitation are common emotional symptoms in oxycodone addiction, particularly during periods of withdrawal or when the drug is unavailable. The central nervous system becomes reliant on the drug to regulate mood, and without it, users experience heightened levels of anxiety, restlessness, and panic. A study by Pergolizzi JV et al. 2020, titled “Opioid withdrawal symptoms, a consequence of chronic opioid use and opioid use disorder: Current understanding and approaches to management,” found that 40-50% of individuals with opioid use disorder experience significant anxiety during withdrawal or when they are unable to access oxycodone.
- Depression: Long-term use of oxycodone alters brain chemistry, particularly affecting serotonin and dopamine levels, which are important for mood regulation. As a result, users develop depression, especially as the body becomes dependent on oxycodone to stabilize mood. A study published in JAMA Psychiatry found that up to 60% of individuals with opioid use disorder experience depressive symptoms, contributing to the emotional toll of addiction.
- Euphoria or extreme mood swings: In the early stages of oxycodone addiction, users experience intense euphoria, which is the result of the drug triggering a massive release of dopamine in the brain. However, as tolerance builds, users experience extreme mood swings, from highs to severe lows. This emotional instability directly results from the brain’s altered reward system. Research by Leung J, Santo T, et al. 2022, titled “Mood and Anxiety Symptoms in Persons Taking Prescription Opioids: A Systematic Review with Meta-Analyses of Longitudinal Studies,” shows that around 75% of people addicted to opioids report experiencing intense mood fluctuations, which worsen over time as the addiction deepens.
What Are the Early Warning Signs of Oxycodone Addiction in Adults?
The early warning signs of Oxycodone addiction in adults are frequent prescription refills, secrecy, changes in daily habits, and an increased focus on obtaining the drug. These signs indicate that a person is beginning to misuse the medication without realizing the severity of their addiction.
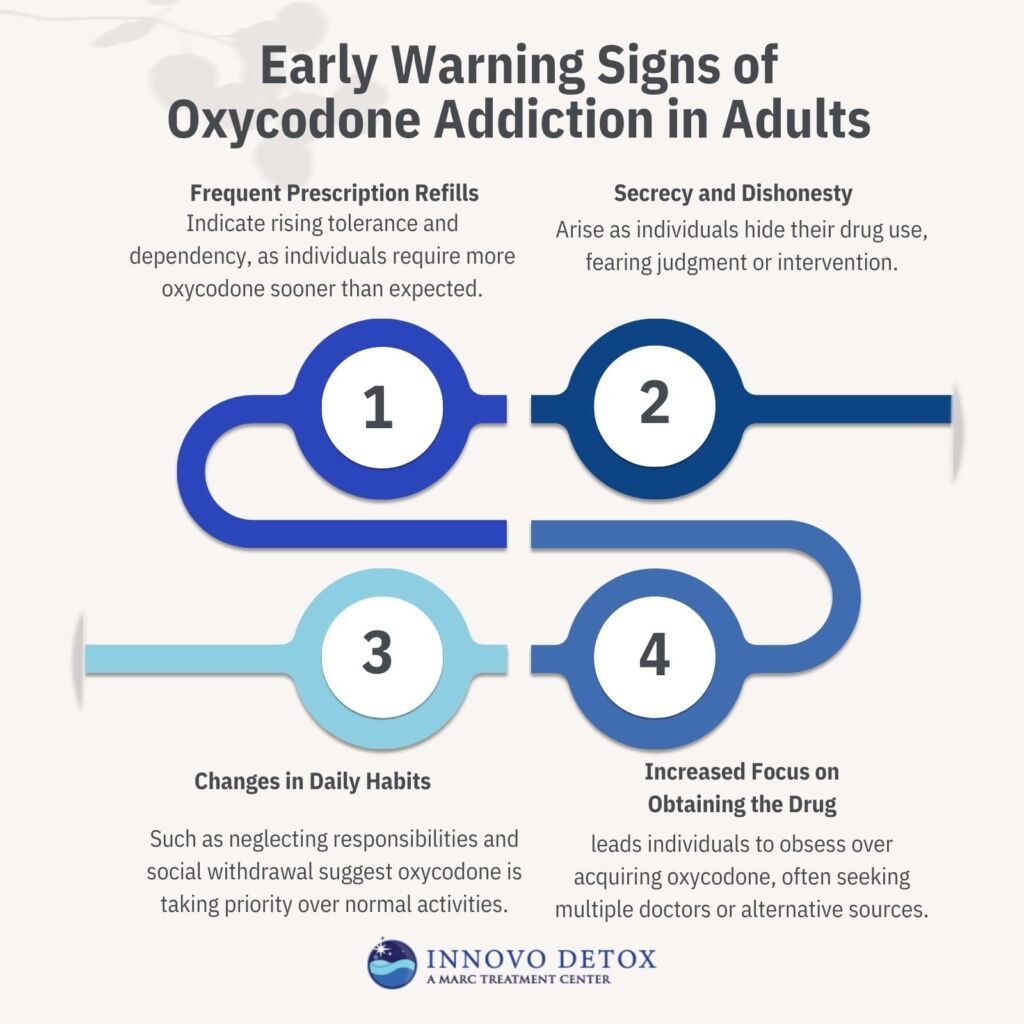
The early warning signs of Oxycodone addiction in adults are as follows:
- Frequent prescription refills: One of the first warning signs of oxycodone addiction is the need for frequent prescription refills. As tolerance to the drug builds, individuals require higher doses to achieve the same effects, prompting them to run out of their prescription sooner than expected. This behavior is a red flag indicating increasing dependence on the drug. Clinical data by the CDC Guideline for Prescribing Opioids for Chronic Pain shows that people with opioid use disorder report needing early refills, signaling a progression toward addiction.
- Secrecy and dishonesty: People struggling with oxycodone addiction become secretive about their drug use, hiding their medication or lying about the amount they are taking. This secrecy stems from guilt or fear of judgment and the desire to maintain their drug use without interference.
- Changes in daily habits: Subtle changes in daily habits, such as neglecting responsibilities, withdrawing from social activities, or a sudden decline in work performance, signal that oxycodone use is becoming problematic. These changes occur because the brain’s reward system is hijacked by the drug, shifting priorities and leading individuals to focus more on obtaining and using oxycodone.
- Increased focus on obtaining the drug: As addiction develops, individuals become preoccupied with obtaining oxycodone, including planning how to acquire more or seeking doctors who will prescribe it. This behavior is driven by the brain’s altered reward system, which begins to prioritize drug use over other activities. Research from the National Institute on Drug Abuse (NIDA) indicates that people with opioid addiction report constant thoughts or actions centered on securing more of the drug.
What Are the Effects of Oxycodone Addiction?
The effects of Oxycodone addiction are drowsiness, nausea, and impaired judgment, along with some long-term effects like severe health issues such as liver damage, respiratory depression, and increased risk of overdose. Short-term effects include drowsiness, nausea, and impaired cognitive function, while long-term abuse results in life-threatening conditions like respiratory depression and liver damage. Addiction disrupts relationships, finances, and societal stability, making it a widespread public health concern.

The effects of oxycodone addiction are as follows:
- Drowsiness: Oxycodone acts as a central nervous system depressant, slowing brain activity and causing excessive drowsiness. This effect results from the drug binding to opioid receptors in the brain, reducing pain perception and inducing sedation. While drowsiness may seem mild, it impairs daily activities, increasing the risk of accidents.
- Nausea and Vomiting: Many opioid users experience nausea due to oxycodone’s effect on the gastrointestinal system. The drug slows digestion, triggering an imbalance in the stomach and brain’s communication pathways, leading to nausea and vomiting. This side effect is common but becomes severe if dehydration or malnutrition occurs.
- Impaired Judgment and Cognitive Function: Oxycodone affects brain chemistry, altering neurotransmitter activity responsible for decision-making and impulse control. As a result, individuals engage in risky behaviors, such as reckless driving or unsafe financial decisions. Long-term abuse causes lasting cognitive impairment, making recovery more challenging.
- Respiratory Depression: One of the most dangerous effects of respiratory depression occurs when oxycodone suppresses the brain’s ability to regulate breathing. This happens because opioids reduce the responsiveness of the brainstem’s respiratory centers. Severe respiratory depression leads to coma or death, particularly when combined with other depressants like alcohol.
- Liver Damage: Many oxycodone formulations contain acetaminophen, which, when taken in high doses, causes liver toxicity. Acetaminophen overdose is one of the leading causes of acute liver failure in the U.S. Chronic oxycodone abuse, even without acetaminophen, contributes to systemic organ stress, worsening liver health.
- Increased Risk of Overdose: Overdose is one of the most dangerous consequences of oxycodone addiction. The drug slows breathing to dangerous levels, leading to hypoxia, brain damage, or death. In 2020, opioid overdoses caused 16,416 deaths, though this number declined to 14,716 in 2022 due to increased awareness and availability of naloxone.
- Financial Instability: Sustaining an oxycodone addiction is costly, with individuals often spending hundreds or thousands of dollars per month on the drug. Financial instability arises as users prioritize drug purchases over essential expenses, leading to mounting debt, job loss, or even criminal activities to fund their addiction.
- Strained Relationships: Addiction affects personal and professional relationships, as individuals become secretive, withdrawn, or dishonest. Families struggle with trust issues while work performance deteriorates, leading to job loss. Many users isolate themselves, worsening their addiction and making recovery more difficult.
- Societal Impact: The opioid epidemic has strained healthcare systems, increased crime rates, and led to lost productivity in the workforce. The financial burden of opioid-related hospitalizations and law enforcement efforts costs billions annually. Oxycodone addiction affects not just individuals but entire communities, emphasizing the need for comprehensive treatment solutions.
What Are Treatment Options for Oxycodone Addiction?
Treatment options for Oxycodone addiction are medical detoxification, medication-assisted treatment (MAT), behavioral therapies, inpatient vs. outpatient programs, and 12-step programs. Each option helps individuals achieve and maintain recovery, depending on their specific needs.

Treatment options for Oxycodone addiction are as follows:
1. Medical Detoxification
Medical detoxification is the first step in recovery from Oxycodone addiction and focuses on safely managing withdrawal symptoms under medical supervision. Detoxification helps individuals manage the physical symptoms of withdrawal, such as anxiety, sweating, nausea, and muscle pain, which are severe and even life-threatening if left untreated.
Healthcare providers monitor vital signs during medical detox and provide medications to ease discomfort and prevent complications. The process is important for stabilizing the individual before continuing with further treatment. Detoxification lasts between 7–10 days, depending on the severity of addiction and individual health. According to SAMHSA, 68% of people who complete drug and alcohol detox programs report their treatment to be successful.
2. Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) is a key intervention for managing Oxycodone addiction, using medications such as methadone, buprenorphine, and naltrexone to reduce cravings and withdrawal symptoms. Methadone and buprenorphine are opioids themselves but are used in controlled doses to mitigate withdrawal effects and cravings without producing the same high as oxycodone.
Naltrexone, an opioid antagonist, blocks the effects of opioids and helps prevent relapse. MAT supports long-term recovery by addressing the brain chemistry altered by addiction, reducing the risk of relapse, and improving overall retention in treatment programs. MAT significantly increases recovery success rates. A study by Feelemyer J et al. 2014, titled “Retention of participants in medication-assisted programs in low- and middle-income countries: an international systematic review,” has found that MAT reduces opioid use by 50% and improves retention in treatment.
According to a study by Kleber HD. et al. 2007, titled “Pharmacologic treatments for opioid dependence: detoxification and maintenance options,” inpatient methadone substitution and taper is usually accomplished in 5 to 7 days and has a retention rate of 80%; with outpatient detoxification, it takes longer to minimize withdrawal symptoms and to decrease dropout and relapse, but only about 20% complete it.
3. Behavioral Therapies
Behavioral therapies treat Oxycodone addiction by addressing the underlying causes and psychological aspects of addiction. Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) help individuals identify and change maladaptive thought patterns and behaviors that contribute to drug use. Group therapy allows individuals to share experiences and learn from others in a supportive environment.
CBT, in particular, has shown strong success rates in treating opioid addiction, with research by McHugh RK et al. 2024, titled “Cognitive behavioral therapy for anxiety and opioid use disorder: Development and pilot testing,” indicating that it leads to a 40 to 60% reduction in opioid use for participants. These therapies focus on developing healthier coping mechanisms, improving emotional regulation, and promoting long-term behavioral changes necessary for sustained recovery.
4. Inpatient vs. Outpatient Treatment
Inpatient and outpatient treatment programs for Oxycodone addiction offer distinct benefits, depending on the severity of the addiction and the individual’s needs. Inpatient treatment provides intensive, structured care in a residential facility, offering 24/7 supervision and support. This setting is especially beneficial for individuals with severe addiction or those who have relapsed multiple times. It provides a highly supportive environment where individuals focus entirely on recovery, away from potential triggers.
Outpatient treatment is more flexible, allowing individuals to live at home while attending therapy and counseling sessions. Outpatient programs are more suitable for those with a stable home environment or those in the early stages of addiction. Research by the Substance Abuse and Mental Health Services Administration (SAMSHA) suggests that inpatient treatment leads to higher retention rates and better outcomes for individuals with more severe addiction. In contrast, outpatient treatment is effective for those with less intense dependencies.
5. 12-Step Program
The 12-step Program, exemplified by programs like Narcotics Anonymous (NA), is a cornerstone of addiction treatment, offering a structured path to recovery through community support and spiritual elements. The program encourages participants to admit their addiction, seek help from a higher power, and engage in regular meetings to share experiences and provide mutual support.
The sense of community encourages accountability and social connection, which are necessary for long-term sobriety. A study by Costello MJ et al. 2019, titled “Effects of 12-step mutual support and professional outpatient services on short-term substance use outcomes among adults who received inpatient treatment,” found that 12-step programs have a significant impact on recovery outcomes, with approximately 33% of participants maintaining sobriety after a year of involvement. These programs emphasize the importance of spiritual recovery, personal growth, and continuous support, which contribute to sustained recovery from Oxycodone addiction.
Can Oxycodone Addiction Be Fully Cured?
No, Oxycodone addiction cannot be fully cured, as it is considered a chronic condition. While individuals achieve long-term sobriety, addiction requires ongoing management and treatment. With the proper support, including therapy, medication-assisted treatment, and relapse prevention strategies, individuals successfully live without active addiction. Experts agree that addiction is a lifelong journey that is effectively managed with continuous care.
How Long Does Oxycodone Addiction Treatment Take?
Oxycodone addiction treatment takes 3 to 6 months, depending on the severity of the addiction and the type of treatment program. Some individuals require longer stays, especially if they are undergoing inpatient care or dealing with long-term addiction. According to treatment guidelines from the Substance Abuse and Mental Health Services Administration (SAMHSA), outpatient programs take 12 weeks, while residential treatment extends beyond 6 months if needed. The duration varies based on individual progress, the presence of co-occurring mental health conditions, and the level of support available after treatment. More extended treatment periods lead to better recovery outcomes, with continuous engagement in support programs.
What Percent of Individuals with Oxycodone Addiction Recover?
Approximately 75% (3 out of 4 people) of individuals with Oxycodone addiction recover, according to research from the CDC. According to the National Institute on Drug Abuse (2021), those who engage in comprehensive treatment programs, particularly those that involve long-term therapy and support, have significantly higher recovery rates. Recovery outcomes improve with ongoing care and the right interventions, and many individuals achieve lasting sobriety.
What Are Effective Relapse Prevention Strategies for Oxycodone Addiction?
Effective relapse prevention strategies for Oxycodone addiction are trigger avoidance, therapy, support groups, and lifestyle changes. These strategies are necessary for maintaining long-term sobriety and preventing a return to substance use. Individuals reduce the risk of relapse and strengthen their recovery by incorporating coping mechanisms, social support, and daily habits that promote wellness.
Effective relapse prevention strategies for Oxycodone addiction are as follows:
- Trigger avoidance: Identifying and avoiding triggers, such as people, places, or situations that prompt cravings, is an important first step in relapse prevention. Developing awareness of these triggers and creating strategies to avoid them helps individuals maintain control. Coping strategies, such as mindfulness or distraction techniques, are used when faced with potential triggers, reducing the likelihood of relapse. Research by the American Journal of Psychiatry shows that individuals who proactively manage triggers are 30-40% less likely to relapse.
- Therapy: Regular therapy, including Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT), is important in addressing the underlying psychological issues that contribute to addiction. Therapy helps individuals develop coping skills to deal with stress, anxiety, and other challenges that might otherwise lead to relapse. CBT, in particular, is highly effective in teaching individuals how to change negative thought patterns and behaviors associated with drug use. According to the National Institute on Drug Abuse (NIDA), therapy reduces the risk of relapse by 50-60% when combined with other treatment modalities.
- Support groups: Engaging in support groups, such as Narcotics Anonymous (NA) or other peer-led programs, provides a sense of community and shared experience. Support groups help individuals stay accountable, reduce isolation, and offer encouragement during difficult times. Social support is necessary for long-term recovery, and research by the Substance Abuse and Mental Health Services Administration (SAMSHA) shows that 12-step groups improve sobriety rates by up to 40% when individuals attend regularly.
- Lifestyle changes: Positive lifestyle changes, such as adopting healthy habits, regular exercise, and good nutrition, help individuals maintain sobriety. A stable routine that includes work, hobbies, and social activities provides structure and reduces the risk of boredom or stress-related relapse. Incorporating healthy habits into daily life also improves mental health, making individuals more resilient to recovery challenges.
What Are the Risks of Relapse After Oxycodone Addiction Treatment?
Relapse risks after oxycodone addiction treatment include exposure to triggers, high levels of stress, and insufficient aftercare. Common triggers, such as environmental cues, negative emotions, or peer pressure, prompt cravings and lead to relapse if not properly managed. Stress, whether due to work, relationships, or other life challenges, also overwhelms individuals and reduces their ability to cope with temptation.
The lack of ongoing support or aftercare programs, such as outpatient therapy or support groups, increases the likelihood of relapse. According to WebMD, relapse rates for opioid addiction are as high as 40-60% within the first year after treatment.
How Do Family Dynamics Influence Recovery From Oxycodone Addiction?
Family dynamics influence recovery from oxycodone addiction by either supporting or hindering the individual’s progress. Family support significantly enhances recovery, as those with strong, positive family relationships are more likely to engage in treatment and stay sober. On the other hand, dysfunctional family dynamics, including enabling behaviors or a lack of understanding, impede recovery.
Family therapy is an important tool in addressing these issues, as it helps to strengthen communication, resolve conflicts, and reduce enabling behaviors. A study by Islam MF, Guerrero M, et al. 2023, titled “The Importance of Social Support in Recovery Populations: Toward a Multilevel Understanding,” shows that individuals with strong family support systems are 50% more likely to complete treatment successfully and maintain long-term recovery. Family involvement is integral for creating a healthy, supportive environment that promotes lasting recovery.
How Can You Support a Loved One Struggling with Oxycodone Addiction?
You can support a loved one struggling with Oxycodone addiction by attending therapy sessions, setting boundaries, and getting professional help for Oxycodone addiction. These strategies provide emotional support, encourage accountability, and ensure access to resources necessary for recovery. A compassionate yet structured approach helps your loved one feel supported while maintaining focus on their treatment journey.
You can support a loved one struggling with Oxycodone addiction by following the below-mentioned strategies:
- Attend therapy sessions: Family or joint therapy sessions strengthen communication and provide a safe space to address underlying issues. Therapy helps both the individual and their loved ones understand the addiction, develop coping skills, and foster a supportive environment.
- Set boundaries: Establishing clear and healthy boundaries is important to prevent enabling behaviors. While it’s necessary to show empathy and support, avoid actions that inadvertently facilitate drug use, such as providing money or covering up for addictive behaviors. Setting boundaries helps promote responsibility and accountability, which are imperative for recovery.
- Seek professional help: Encourage your loved one to access professional help for Oxycodone addiction, such as medical detox and therapy. Professional services offer evidence-based interventions and a structured recovery plan. It ensures that your loved one receives the specialized care they need to address their addiction effectively.
- Be patient and supportive: Recovery is a long-term process that requires persistence and understanding. Offer encouragement during setbacks and celebrate small victories to motivate your loved one. Emotional support from close friends and family members significantly impacts their willingness to stay committed to recovery.
Which Local Resources Are Available in Pennsylvania for Oxycodone Addiction Treatment?
Local resources that are available in Pennsylvania for Oxycodone addiction treatment include state-funded programs, specialized treatment centers, and community support services. These resources offer comprehensive care options to assist individuals in overcoming addiction and achieving long-term recovery.
Local resources that are available in Pennsylvania for Oxycodone addiction treatment are as follows:
- Pennsylvania Department of Drug and Alcohol Programs (DDAP): The DDAP provides information on substance use disorder treatment services across the state. Individuals seeking help can call the 24/7 hotline at 1-800-662-HELP to connect with local treatment options and support services.
- Pennsylvania Opioid Misuse and Addiction Abatement Trust: This organization manages funds from opioid settlements to support addiction treatment and prevention programs across the state, enhancing the availability of resources for those in need.
How Can Adults Safeguard Against Oxycodone Misuse?
Adults can safeguard against oxycodone misuse by using prescriptions precisely as directed, avoiding sharing medications and exploring alternative treatments for pain management. Proper prescription use involves following the dosage and duration recommended by healthcare providers and promptly disposing of unused medication to prevent misuse. Sharing medications is a common yet dangerous practice that increases the risk of addiction and overdose.
Exploring non-opioid pain management alternatives, such as physical therapy, acupuncture, or over-the-counter medications, helps reduce reliance on oxycodone. According to the Centers for Disease Control and Prevention (CDC), these practices are key components of opioid safety and significantly reduce the likelihood of misuse and addiction.
What Are Alternative Pain Management Options to Oxycodone?
Alternative pain management options to oxycodone include physical therapy, acupuncture, and over-the-counter medications. These non-opioid alternatives provide effective pain relief while reducing the risk of dependency and side effects associated with opioids. Physical therapy helps improve mobility and relieve pain through targeted exercises, while acupuncture has been shown to alleviate chronic pain by stimulating the nervous system.
Over-the-counter medications, such as acetaminophen and ibuprofen, are effective for managing mild to moderate pain. Research by Lin JG, Chan YY, Chen YH. et al. 2012, titled “Acupuncture for the treatment of opiate addiction,” shows that acupuncture reduces cravings and improves treatment retention rates, primarily when used alongside traditional therapies.
How Addictive Is Oxycodone Compared to Other Prescribed Painkillers?
Oxycodone is highly addictive compared to other prescribed painkillers, ranking among the most potent and commonly misused opioids. While it is less powerful than fentanyl, it is more addictive than codeine and morphine due to its fast onset of action and euphoric effects.
A study by the Journal of Addiction Medicine indicates that oxycodone has a higher misuse potential than hydrocodone, with dependence rates estimated at around 26% for long-term users, compared to 23% for hydrocodone and 14% for codeine. These differences in addiction risk are influenced by oxycodone’s pharmacological properties, including its ability to bind strongly to opioid receptors, creating a rapid and intense reward system in the brain.
What Are Common Withdrawal Symptoms of Oxycodone?
Common withdrawal symptoms of Oxycodone are nausea, anxiety, sweating, and intense cravings. These symptoms occur as the body reacts to the sudden absence of the drug, which it has become dependent on to regulate certain functions. The severity of these symptoms varies based on the duration and dosage of Oxycodone use, requiring medical support for safe management.
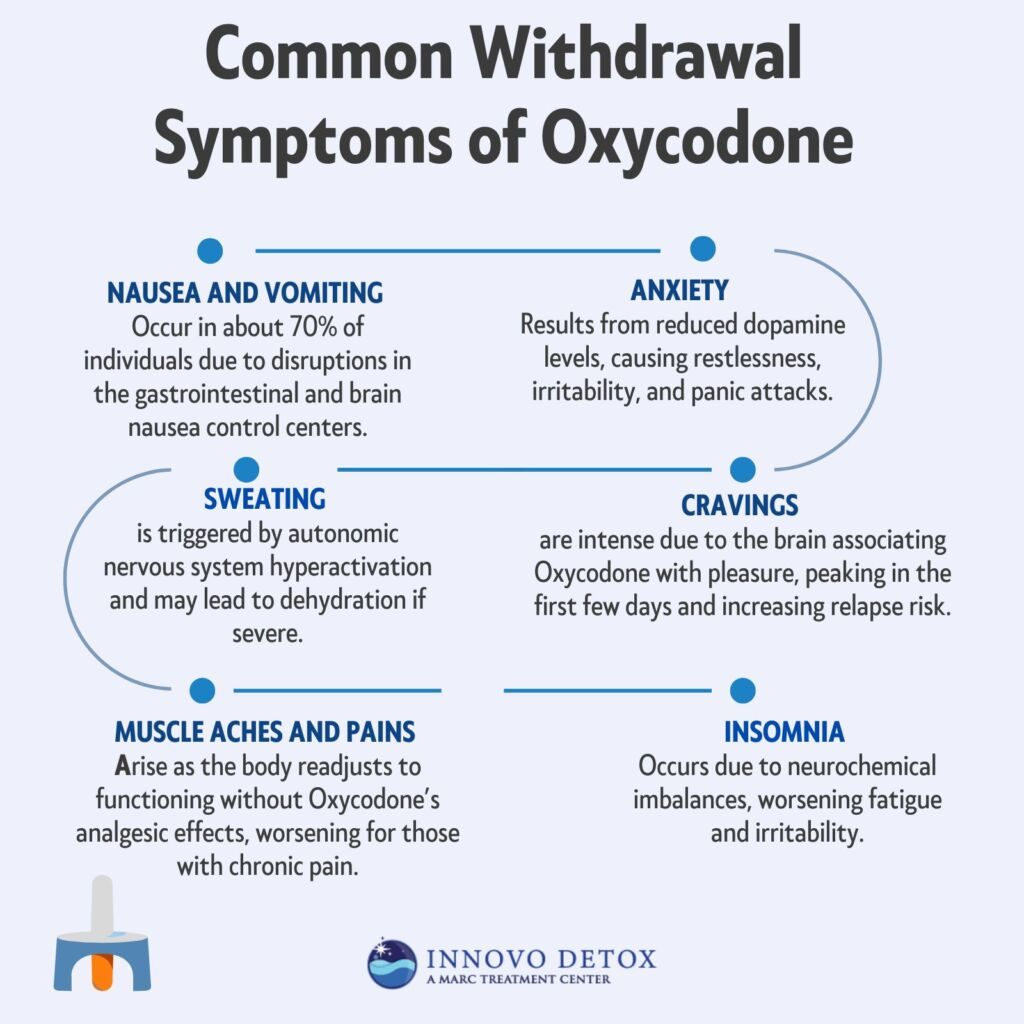
Common withdrawal symptoms of Oxycodone are as follows:
- Nausea and vomiting: Nausea is a frequent withdrawal symptom caused by the drug’s impact on the gastrointestinal tract and the brain’s nausea control centers. This symptom ranges from mild discomfort to severe vomiting and is experienced by approximately 70% of individuals undergoing opioid withdrawal, according to a study by Shah M, Huecker MR. et al. 2023, titled “Opioid Withdrawal.”
- Anxiety: Anxiety during withdrawal stems from disruptions in the brain’s reward and stress regulation systems, particularly the decreased production of dopamine. It manifests as restlessness, irritability, or panic attacks and affects most individuals withdrawing from opioids.
- Sweating: Profuse sweating is a common physical symptom caused by the hyperactivation of the autonomic nervous system in response to the absence of Oxycodone. Chills accompany it, and if severe, they lead to dehydration.
- Cravings: Intense cravings for Oxycodone occur due to the brain’s association of the drug with pleasure and relief. These cravings are among the most challenging withdrawal symptoms and are a significant risk factor for relapse. Cravings peak within the first few days of withdrawal and gradually decline over time.
- Muscle aches and pains: Oxycodone withdrawal causes generalized muscle discomfort due to the body’s attempt to regain normal function without the drug’s analgesic effects. This symptom is particularly distressing in individuals with underlying chronic pain.
- Insomnia: Difficulty sleeping is common during withdrawal as the brain’s neurochemical balance is disrupted. Insomnia further exacerbates other withdrawal symptoms, such as fatigue and irritability.
How Does Oxycodone Addiction Differ Between Men and Women?
Oxycodone addiction differs between men and women in prevalence, psychiatric comorbidity, self-administration patterns, and response to treatment. Men are statistically more likely to misuse Oxycodone, while women develop dependence more quickly due to biological and hormonal factors. Women are also more likely to experience co-occurring mental health issues, such as anxiety and depression, which complicate addiction.
Oxycodone addiction differs between men and women in the following ways:
- Prevalence: Men are generally more likely to misuse Oxycodone and other opioids, with the National Institute on Drug Abuse showing higher rates of prescription drugs. Women are more likely to be prescribed opioids for chronic pain and are at greater risk of developing dependency due to higher pain sensitivity and hormonal influences. These differences reflect varying societal and medical approaches to pain management by gender.
- Psychiatric Comorbidity: Women with Oxycodone addiction are more likely to experience co-occurring mental health conditions such as anxiety, depression, and post-traumatic stress disorder (PTSD). Research in the Journal of Substance Abuse Treatment found that women with opioid use disorder have a 50% higher likelihood of depression compared to men, which exacerbates their addiction and complicates treatment outcomes.
- Self-Administration Patterns: Women begin using Oxycodone for pain management and escalate their usage due to emotional distress. At the same time, men are more likely to misuse the drug for recreational purposes or euphoria. These patterns indicate that psychological and emotional triggers addiction for women, while behavioral factors are more prominent for men.
Response to Treatment: Women tend to respond better to treatments incorporating counseling and behavioral therapies addressing emotional and psychological factors. Men benefit from structured, goal-oriented programs that address behavioral patterns. A study published in Addiction Science & Clinical Practice highlighted that gender-specific treatment approaches improved outcomes for both men and women.